Candidaemia is the presence of Candida spp. in blood, diagnosed with a positive blood culture. It should always be taken seriously as it is only very rarely insignificant. Candida spp. are usually opportunists, exploiting some underlying defect in the patients immunity to infection. The most common sources of infection are:
• Central Venous Catheters (CVC)
• Intra-abdominal infections, perforation or abscesses
• Urinary tract infections, particularly if prosthetic material is present e.g. catheters or ureteric stents
• Intravascular infections associated with prosthetic material e.g. infective endocarditis, vascular grafts
Candidaemia should be considered in any patient with a serious abdominal problem or intravascular or urinary tract prosthetic material e.g. CVC or urinary tract stents, especially if they are immunosuppressed.
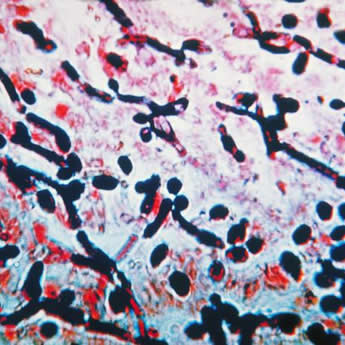
Strictly speaking Candida spp. are facultative anaerobes, they grow both aerobically and anaerobically. In practice they grow much better in the aerobic blood culture bottles but they are relatively slow growing. Most significant bacteria will grow within 24 hours of incubating a blood culture, but Candida spp. (a fungus) tend to take 48 hours and sometimes even longer. They can also be very tricky to spot in the Gram film as there is often not much microorganism present. One tip for spotting them in a Gram film is if you cannot see anything obvious at high power (x1000) then switch to low power (x100) and scan the film, the fungal hyphae will be easy to spot as a clump of regularly shaped Gram-positive material which resolves into the typical Gram-positive appearance when you switch back to high power.
First line treatment for candidaemia is an echinocandin e.g. Caspofungin, Anidulafungin or Micafungin. There is little to choose between the types; my preference is for Caspofungin as it has been around longer and there is more evidence for its use, NB I have no vested interest in any pharmaceutical company.
The normal dose of IV Caspofungin is:
• 70mg on the first day then 50mg OD afterwards
• If the patient is 80kg or more the daily dose should be increased to 70mg OD
• If the patient is in liver failure the dose will need reducing
• There is no adjustment necessary for renal failure
Caspofungin is very active against Candida spp. in biofilms which is an advantage when dealing with the long-term management of endocarditis, see below.
Second line treatment is usually an IV lipid formulation of Amphotericin B (e.g. AmBisome, Abelcet) at a dose of 1mg/kg. Amphotericin B is very broad spectrum but it doesn’t treat C. lusitaniae which is resistant. If treating C. lusitaniae and an echinocandin can’t be used then consider using an azole like Fluconazole, Voriconazole or Posaconazole.
Why not use Fluconazole empirically to treat candidaemia? Fluconazole is a lot cheaper but there are a number of reasons why not:
1. Fluconazole is a candistatic agent not candicidal whereas echinocandins and Amphotericin B are candicidal
2. Fluconazole is not active against all types of common Candida spp. (C. krusei and C. glabrata are often resistant)
Fluconazole might be the treatment of choice for C. parapsilosis as it is more active in vitro against this species, but this should only be used if the identification is certain.
All candidaemia isolates should have antifungal sensitivities performed to help guide ongoing treatment. This is a reference laboratory test in the UK.
• Source unknown – at least 2 weeks, but keep trying to find the source
• CVC – 2 weeks with removal of CVC
• Intra-abdominal – 2 weeks if removal of source (e.g. complete drainage of abscess) otherwise 4 weeks
• UTI – at least 2 weeks, up to 4-6 weeks if fungal balls present (seen on ultrasound scan)
• Intravascular – at least 6 weeks with removal of intravascular prosthetic material, may require lifelong suppression therapy with oral antifungal afterwards
Candida spp. are very good at colonising prosthetic material. If the patient has prosthetic material in their blood stream it is very likely that it will have been colonised within 12 hours of the onset of candidaemia. The most common intravascular material in these patients are CVCs and so it is recommended that all candidaemic patients have their lines changed after starting antifungal treatment. There is no point changing the lines before starting treatment as the new lines will become colonised just as quickly as the old ones unless there is antifungal present to prevent this occurring. My personal practice is to try and wait for 24-48 hours after starting treatment before changing the lines.
Ensure treatment is effective and look for secondary infections
All patients who have candidaemia should have further investigations to look for a source and to look for secondary infections. These include:
Repeat blood cultures at 48 hours
This not only assesses the effectiveness of treatment but if positive suggests that the patient either has an intravascular infection or a large abscess both of which might need surgical intervention.
Echocardiography
An Echo should be done to look for both primary and secondary infective endocarditis. Even if a patient didn’t originally have an infected heart valve, it is not uncommon for a candidaemia to result in endocarditis as a result of the Candida spp. seeding the heart valve.
Candida endocarditis is very difficult to treat, usually requiring surgical replacement of the heart valve, a minimum of 6 weeks IV antifungals and then lifelong antifungal suppression as the infection is very rarely cleared.
In the future, echinocandins may be shown to cure Candida endocarditis completely because of their enhanced effect against Candida spp. in biofilms (the vegetation on the heart valve is essentially a biofilm; a collection of microorganisms sticking to a surface)
Ophthalmology assessment
Candidaemia can result in Candida endophthalmitis or retinitis as a secondary infection and therefore all patients with candidaemia should be seen within the first few days by an experienced ophthalmologist. Treatment is difficult and failure to diagnose infection early or treat successfully results in loss of vision or the need to remove the eye. Treatment is at least 6 weeks of IV therapy using combinations of antifungals, often also involving injecting antifungals directly into the eye.
Neonates
Premature neonates often disseminate Candida spp. to most body tissues when they are candidaemic, including the central nervous system and the urinary tract. Candida meningitis and fungal balls in the kidneys are common. Treatment is complicated, requiring a minimum of 6 weeks of antifungals in my experience, although some guidelines suggest 3 weeks may be enough in uncomplicated infections where dissemination has not occurred.
So candidaemia is not really that difficult to know how to manage. The 3 key aspects are:
- Make the diagnosis
- Treat the infection
- Ensure treatment is effective and look for secondary infections
However, it is also important to keep in mind that management of candidaemia is not always successful, even if you do everything right.
Do you have a topic which you would like me to blog about? Either post a comment or email me via the contact page and I will try and accommodate as many requests as possible.

 RSS Feed
RSS Feed
