Community Acquired Pneumonia (CAP)
Community acquired pneumonia (CAP) is an acute infection of lung tissue with onset outside of hospital or within 48 hours of admission to hospital.
The NICE guidelines suggest that patients from nursing homes should be treated as CAP, however this disregards the level of care the resident is receiving. Some would argue that those who receive a level of nursing care equivalent to that received in hospital should be treated as hospital acquired pneumonia rather than CAP because they have a different normal flora (see section – Basic Concepts, Bacterial Flora in a Normal Person in a Hospital or Long-term Care Facility).
The British Thoracic Society Definitions for diagnosis are:
The NICE guidelines suggest that patients from nursing homes should be treated as CAP, however this disregards the level of care the resident is receiving. Some would argue that those who receive a level of nursing care equivalent to that received in hospital should be treated as hospital acquired pneumonia rather than CAP because they have a different normal flora (see section – Basic Concepts, Bacterial Flora in a Normal Person in a Hospital or Long-term Care Facility).
The British Thoracic Society Definitions for diagnosis are:
In community |
|
In hospital (<48 hours) |
|
Clinical Features
Respiratory symptoms and signs• Cough
• Shortness of breath • Purulent sputum • Chest pain • Chest signs of consolidation - Reduced chest movement - Dull percussion - Bronchial breathing - Increased tactile vocal fremitus & vocal resonance |
Systemic symptoms• Fever
• Sweats • Shivers • Aches • Pains |
In Children• Fever
• Increased respiratory rate • Cough • Recession • Chest pain or pain referred to abdomen |
Assessment of Severity
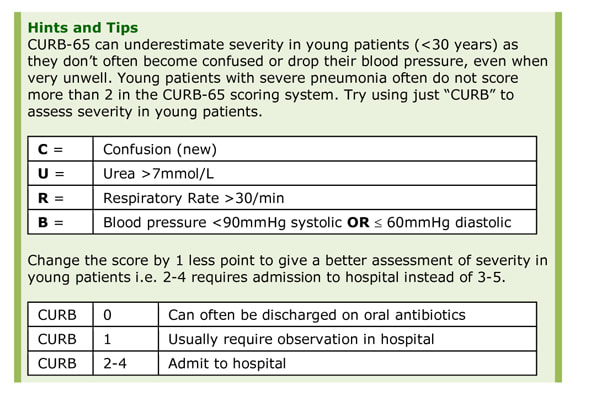
C = Confusion (new)
U = Urea >7mmol/L
R = Respiratory Rate >30/min
B = Blood pressure <90mmHg systolic OR 60mmHg diastolic
65 = Age >65 years
Score = 1 each per criteria e.g. C + R + >65 = 3
C = Confusion (new)
U = Urea >7mmol/L
R = Respiratory Rate >30/min
B = Blood pressure <90mmHg systolic OR 60mmHg diastolic
65 = Age >65 years
Score = 1 each per criteria e.g. C + R + >65 = 3
|
CURB-65 = 0-1
CURB-65 = 2 CURB-65 = 3-5 |
Can often be discharged on oral antibiotics
Usually require observation in hospital Usually require admission to hospital |
In primary care the CURB-65 score can be modified to a CRB-65 score (without urea) to assess risk of death and whether to admit to hospital:
|
CURB-65 = 0
CURB-65 = 1-2 CURB-65 = 3-4 |
1% mortality, manage at home
1-10% mortality, consider admitting to hospital >10% mortality, admit to hospital |
When CURB-65 was introduced (1996) elderly care in the UK was >65 years old; an age previously associated with worsening health. Frailty, rather than age, may now be a better indicator as CURB-65 overestimates severity in some otherwise healthy over 65 year olds e.g. some 70 year olds are treated with IV antibiotics when they should really be given orals and sent home.
Causes
Common
If history of COPD, as above plus:
• Pseudomonas aeruginosa
If aspiration, as above plus:
• Anaerobes e.g. Bacteroides sp., Fusobacterium sp.
If zoonotic
• Chlamydiapsittaci (from parrots and budgerigars)
If empyema
• Staphylococcus aureus
• Streptococcus pneumoniae
• Streptococcus anginosus group
- Staphylococcus aureus
- Streptococcus pneumoniae
- Haemophilus influenzae
- Mycoplasma pneumoniae
- Legionella pneumophila (especially if travelled)
- Chlamydia pneumoniae
- Viral e.g. Influenza Virus, Parainfluenza Virus, Respiratory Syncytial Virus (RSV), Adenovirus
If history of COPD, as above plus:
• Pseudomonas aeruginosa
If aspiration, as above plus:
• Anaerobes e.g. Bacteroides sp., Fusobacterium sp.
If zoonotic
• Chlamydiapsittaci (from parrots and budgerigars)
If empyema
• Staphylococcus aureus
• Streptococcus pneumoniae
• Streptococcus anginosus group
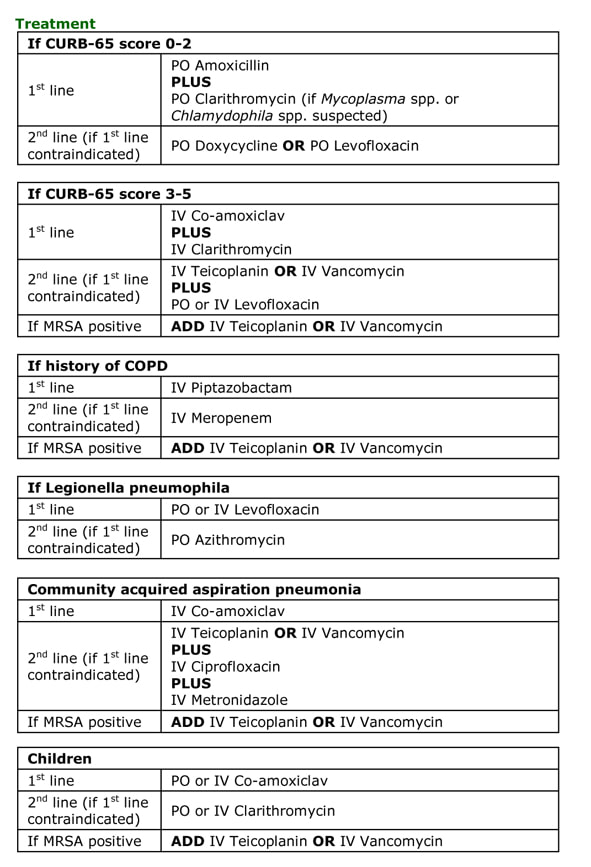
Total Duration
5-7 days
Legionella pneumonia: 7-10 days (14-21 days if immunosuppressed)
Empyema requires drainage and 2-4 weeks total treatment
Dosing
See section - Antibiotics, Empirical Antibiotic Guidelines.
Prognosis and Complications
Mortality is dependent on CURB-65 score:
5-7 days
Legionella pneumonia: 7-10 days (14-21 days if immunosuppressed)
Empyema requires drainage and 2-4 weeks total treatment
Dosing
See section - Antibiotics, Empirical Antibiotic Guidelines.
Prognosis and Complications
Mortality is dependent on CURB-65 score:
|
CURB-65 0-1
CURB-65 2 CURB-65 3-5 |
<3%
9% 15-40% |
Up to 40% of patients with Streptococcus pneumoniae reactivate Herpes Simplex Virus (HSV) leading to cold sores.
Prophylaxis and Prevention
No role for antibiotics to prevent recurrence
Vaccine against Streptococcus pneumoniae:
No role for antibiotics to prevent recurrence
Vaccine against Streptococcus pneumoniae:
- 23-valent (adults) covers approximately 96% of pneumonia strains but not active in <2 year olds
- 13-valent (children) covers approximately 90% of pneumonia strains
- Vaccination of children reduces exposure and hence infection in adults by decreasing reservoir of bacteria in community
Topics in Clinical Scenarios - Respiratory Infections:
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).
- Community Acquired Pneumonia (CAP)
- Aspiration Pneumonia
- Hospital Acquired Pneumonia (HAP)
- Ventilator Associated Pneumonia (VAP)
- Infective Exacerbation of COPD
- Acute Bronchitis
- Upper Respiratory Tract Infection (URTI)
- Influenza
- Tuberculosis (TB)
- Multidrug Resistant TB (MDR TB) and Extensively Drug Resistant TB (XDR TB)
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).