Meningitis
Meningitis is inflammation of the meninges, the membranes surrounding the brain.
Clinical Features
- Fever
- Headache
- Photophobia
- Neck stiffness
- Pain on extension of the leg (Kernig’s sign)
- Decreased conscious level
- Confusion
- Seizures (30% of patients)
- Focal neurological signs (20% of patients)
Causes
|
Common
If Elderly OR Pregnant As above plus:
|
If Unvaccinated
|
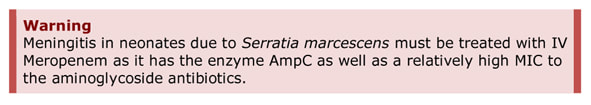
Neonates
- Group B Beta-haemolytic Streptococcus (Streptococcus agalactiae
- Escherichia coli
- Klebsiella sp.
- Salmonella sp.
- Listeria monocytogenes
- Serratia marcesans
- Enterovirus
- Herpes Simplex Virus (HSV)
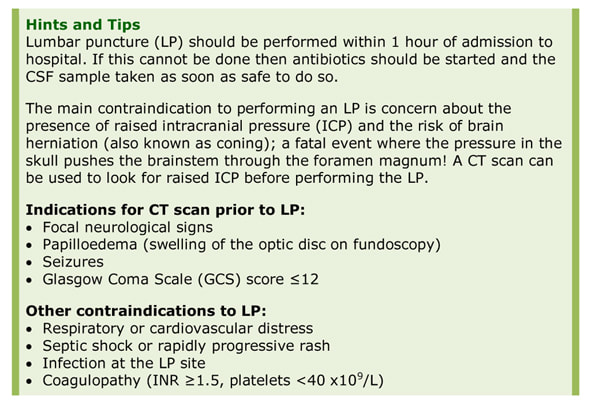
Investigations
- Blood cultures
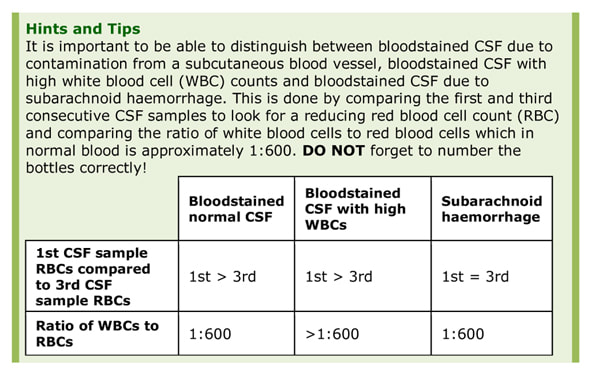
- Cerebrospinal fluid (CSF) for microscopy, culture and sensitivity, glucose and protein
- Peripheral blood glucose to compare to CSF
- EDTA blood for N. meningitidis and Streptococcus pneumoniae PCR
- Bacterial throat swab for N. meningitidis culture
- Viral throat swab and stool for Enterovirus PCR
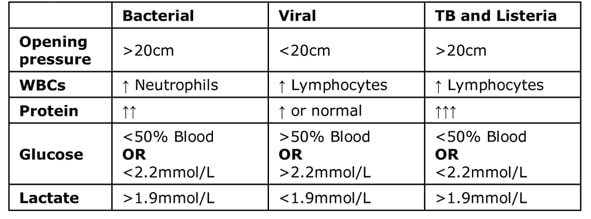
Interpretation of CSF
Bacterial Meningitis Score
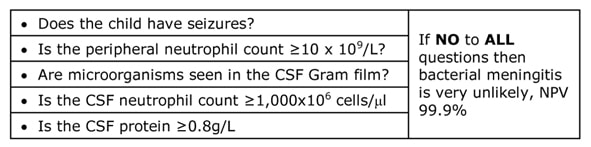
The Bacterial Meningitis Score (BMS) can be used to predict the likelihood of bacterial meningitis. It is validated in children, and may become validated in adults in the future.
The Bacterial Meningitis Score (BMS) can be used to predict the likelihood of bacterial meningitis. It is validated in children, and may become validated in adults in the future.
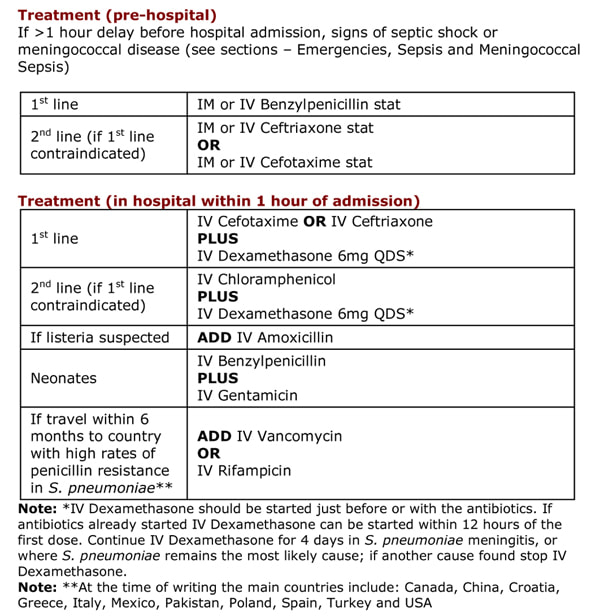
Total Duration
Dosing
See section - Antibiotics, Empirical Antibiotic Guidelines Emergencies.
Prognosis and Complications
Untreated bacterial meningitis has 100% mortality. Even with treatment the mortality from meningitis is 20% (30% with S. pneumoniae or L. monocytogenes). Long-term sequelae including weakness, sensory loss, seizures and cranial nerve abnormalities occur in 44% L. monocytogenes, 30% S. pneumoniae and 7% N. meningitidis.
Viral meningitis is usually a self-limiting infection, which does not require treatment in patients with normal immune systems.
Complications are more common with bacterial rather than viral meningitis and include:
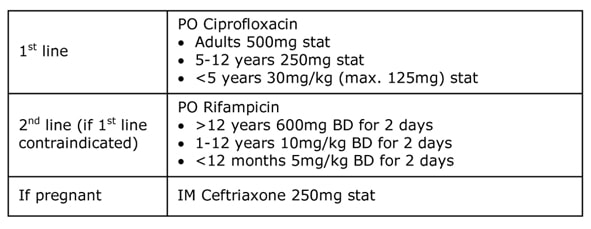
Prevention and Prophylaxis
Many causes of bacterial meningitis can be prevented with the primary course of vaccines, including S. pneumoniae, H. influenzae type b and N. meningitidis types A, B, C, W and Y.
Prophylactic antibiotics are usually given to close contacts, within the previous 7 days, of patients with N. meningitidis meningitis; vaccinations are also occasionally given. The decision for this lays with the Consultant in Communicable Disease Control (CCDC) or Public Health Consultant, not the admitting doctors. These antibiotics penetrate into the upper respiratory tract and eliminate carriage from those who might have passed the bacterium onto the patient as well as anyone who might have acquired the bacterium from the patient. Any patient treated for N. meningitidis meningitis with Benzylpenicillin alone should be given oropharyngeal decolonisation as for prophylaxis in close contacts below.
- Neisseria meningitidis – 5-7 days
- Streptococcus pneumoniae – 14 days
- Haemophilus influenzae type b - 10 days
- Group B Beta-haemolytic Streptococcus - 14 days
- Listeria monocytogenes - 21 days
- Enterobacteriaceae - 21 days (30% of patients relapse requiring a further 21 days of treatment)
Dosing
See section - Antibiotics, Empirical Antibiotic Guidelines Emergencies.
Prognosis and Complications
Untreated bacterial meningitis has 100% mortality. Even with treatment the mortality from meningitis is 20% (30% with S. pneumoniae or L. monocytogenes). Long-term sequelae including weakness, sensory loss, seizures and cranial nerve abnormalities occur in 44% L. monocytogenes, 30% S. pneumoniae and 7% N. meningitidis.
Viral meningitis is usually a self-limiting infection, which does not require treatment in patients with normal immune systems.
Complications are more common with bacterial rather than viral meningitis and include:
- Subdural empyema
- Seizures
- Cerebral venous sinus thrombosis
Prevention and Prophylaxis
Many causes of bacterial meningitis can be prevented with the primary course of vaccines, including S. pneumoniae, H. influenzae type b and N. meningitidis types A, B, C, W and Y.
Prophylactic antibiotics are usually given to close contacts, within the previous 7 days, of patients with N. meningitidis meningitis; vaccinations are also occasionally given. The decision for this lays with the Consultant in Communicable Disease Control (CCDC) or Public Health Consultant, not the admitting doctors. These antibiotics penetrate into the upper respiratory tract and eliminate carriage from those who might have passed the bacterium onto the patient as well as anyone who might have acquired the bacterium from the patient. Any patient treated for N. meningitidis meningitis with Benzylpenicillin alone should be given oropharyngeal decolonisation as for prophylaxis in close contacts below.
Topics in Clinical Scenarios - Emergencies:
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).
- How to Recognise the Sick Patient
- National Early Warning Score (NEWS)
- Paediatric Early Warning Score (PEWS)
- Sepsis
- Adult Sepsis “Golden-Hour” Management Flowchart
- Neutropaenic Sepsis and Febrile Neutropaenia
- Neutropaenic Sepsis Antibiotic Flowchart
- Toxic Shock Syndrome (TSS)
- Meningitis
- Meningococcal Sepsis
- Initial Management of Bacterial Meningitis and Meningococcal Sepsis in Adults
- Initial Management of Bacterial Meningitis in Children
- Initial Management of Meningococcal Sepsis in Children
- Encephalitis
- Epiglottitis
- Spinal Epidural Abscess
- Necrotising Fasciitis
- Malaria
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).