Diagnosing Infection
It may sound obvious but in order to manage a patient with an infection safely and effectively you first have to work out what is wrong with them. This is done through the dynamic process of formulating a differential diagnosis. The process begins the moment the patient is referred (e.g. you are told the patient has a cough you narrow questioning to the respiratory system and a differential diagnosis that includes diseases like pneumonia, lung cancer, COPD etc). By taking a history, examination and requesting targeted investigations you narrow down the differential diagnosis until you get to a single diagnosis.
A differential diagnosis is a list of potential diseases or infections that a patient might have. The simplest and most effective method of formulating a differentia diagnosis is:
In the History the key infection related aspects to concentrate on are:
In the Examination the key infection related aspects to concentrate on are:
Diagnosing Infection: Non-Microbiological Investigations include:
A differential diagnosis is a list of potential diseases or infections that a patient might have. The simplest and most effective method of formulating a differentia diagnosis is:
- Immediately life threatening conditions e.g. meningitis, encephalitis, necrotising fasciitis
- Common conditions e.g. UTI, pneumonia, cellulitis, heart failure
- Uncommon conditions e.g. infective endocarditis
In the History the key infection related aspects to concentrate on are:
- The patient's specific symptoms - e.g. cough indicating chest or upper respiratory tract or right upper quadrant pain indicating possible cholangitis
- A chronological timeline of when and how symptoms developed - e.g. Chicken Pox followed by haemorrhagic skin lesions pointing towards invasive Group A Beta-haemolytic Streptococcus and necrotising fasciitis
- Contact with people with infections OR symptoms - e.g. Tuberculosis contact
- A list of recent travel (countries and regions) - e.g. Malaria endemic regions
- The patient’s vaccination history - e.g. primary infant courses as well as travel related vaccines
- The patient’s current and former occupations - e.g. healthcare staff and blood borne viruses or plumbers and exposure to Legionella pneumophila
- The patient’s pastimes and hobbies - e.g. water sports and exposure to rats in leptospirosis
- Any pets OR contact with animals - zoonotic infections e.g. Pasteurella multocida and cat bites, Chlamydia psittaci and parrots
- A sexual history - e.g. sexually transmitted diseases and blood borne viruses
- The patient’s ethnic origin - e.g. exposure to relatives with tropical infections
- The patient’s country of birth - e.g. chronic tropical infections or exposure to relatives with tropical infections
In the Examination the key infection related aspects to concentrate on are:
- General observations - e.g. inhalers, bedside medications, finger clubbing, splinter haemorrhages or presence of new onset confusion
- Presence and pattern of fever - e.g hyperthermia (>38°C) OR hypothermia
- (<36°C), Vivax and Ovale malaria fever every 48 hours, Malariae malaria fever every 72 hours, Falciparum malaria fever more frequent than 24 hours
- Heart rate - e.g. tachycardia >90 bpm in sepsis, BEWARE Beta-blockers falsely decrease heart rate OR arrhythmias can falsely increase heart rate
- Blood pressure - e.g. systolic pressure <90mmHg OR decreased >40mmHg from baseline, BEWARE “normotensive” patients may actually be “hypotensive” if they are normally “hypertensive”
- Skin lesions - e.g. blanching and non-blanching rashes can occur in meningococcal sepsis, erythema marginatum occurs in rheumatic fever, BEWARE symptoms more severe than clinical features consider necrotising fasciitis
- Upper respiratory tract - e.g. tonsillar pus and presence of quinsy or swelling and erythema of the tympanic membrane in otitis media
- Chest - e.g. decreased expansion, dullness to percussion, bronchial breathing and increased vocal resonance (tactile vocal fremitus) in consolidation
- Heart - e.g. new murmurs in infective endocarditis, BEWARE if severe valve damage, there may be no murmurs as no turbulence of blood flow
- Abdomen - e.g. right upper quadrant pain in cholangitis or loin pain in pyelonephritis
- Central nervous system - e.g. acute confusion in the elderly (also part of CURB-65 in CAP) or neck stiffness and meningism in meningitis
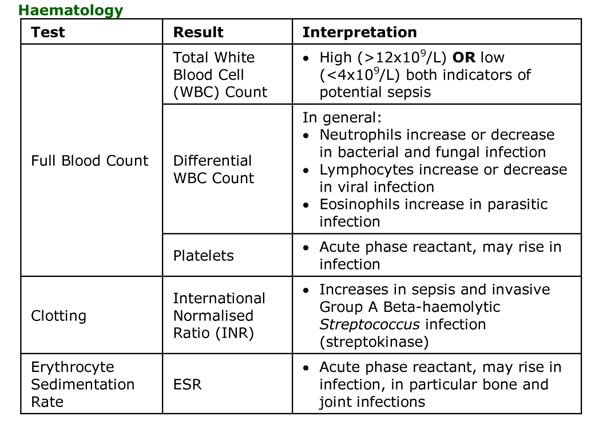
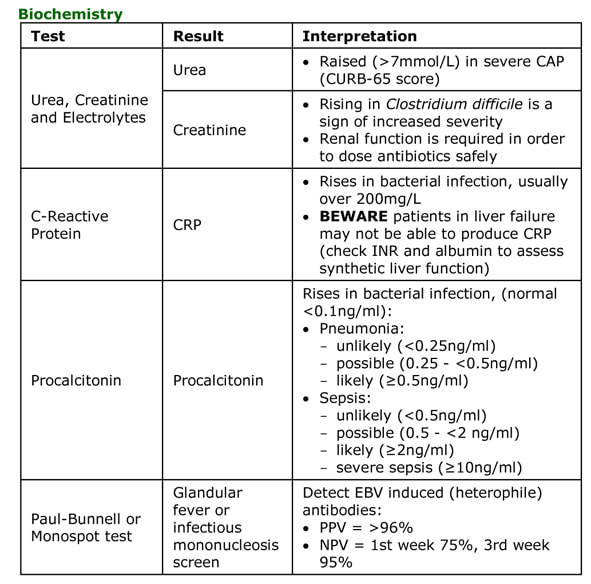
Diagnosing Infection: Non-Microbiological Investigations include:
Topics in Basic Concepts:
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger as its got 1/3 more in it! (11cmx18cmx2.5cm).
- What is Infection? Infection vs. Colonisation vs. Contamination
- Source of Infection: Endogenous vs. Exogenous
- Bacteraemia vs. Septicaemia
- Types of Infectious Microorganisms
- The Anatomy of a Bacterium
- What is Normal Flora and why is it Important?
- Circumstances Affecting Normal Flora
- How Antibiotic Prescribing Influences Normal Flora and the Ward Environment
- Bacterial Flora in a Normal Person in the Community
- Bacterial Flora in a Normal Person in a Hospital or Long-term Care Facility
- Significance of Bacteria in the Bloodstream (Bacteraemia)
- Diagnosing Infection: History
- Diagnosing Infection: Examination and Non-Microbiological Investigations
- Immunodeficiency States
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger as its got 1/3 more in it! (11cmx18cmx2.5cm).