Then a further 4 cases have been diagnosed! Also unrelated to the previous cases and with no obvious source for the infection… however these cases have all occurred in gay or bisexual men who have sex with men (MSM).
This is extremely concerning! We have now had 6 cases of Monkey Pox in people who have not been to Africa and who have no obvious source for the infection. This means we have an unknown source of infection in the UK population. On top of this we now have cases in a group of the population where spread may occur more readily through sexual activity. It is very unlikely that these 7 cases are going to be the last cases identified!
So, time for an update… what has changed since the blog in 2018?
Epidemiology
Monkey Pox is still a rare infection. In the Democratic Republic of the Congo where most cases have been reported, surveillance studies during “outbreaks” have shown an incidence of past infection between 0.001-0.05% of the population, that’s about 1 in 100,000, but that’s when they are looking for cases during an outbreak, not all the time, so the true rate could be lower than this.
There are 2 main types of Monkey Pox, West African and Central African. West African causes a milder infection with a mortality of about 1%; Central African is more severe with a mortality of about 10%. Fortunately for us, the cases in the UK so far have all been the West African type and are therefore mild infections.
Person-to-person transmission is rare, with a household secondary case rate of 8%, but transmission can still occur from touching infective lesions, respiratory droplets and possibly also sexual contact.
Case definition
The current UK case definition for a probable case of Monkey Pox is:
- Symptoms including: fever >38.5oC, headache, myalgia, arthralgia, back pain or lymphadenopathy
- Contact with a case of Monkey Pox within 21 days of symptom onset OR travel to West Africa or Central Africa within 21 days of symptom onset OR MSM
The rash of Monkey Pox is vesicular (small fluid filled blisters) starting 1-5 days after onset of fever. It usually starts on the face or genitalia and then spreads to the rest of the body. It may look similar to chicken pox. Skin lesions eventually scab over, dry and then fall off.
Any patient meeting the case definition should be URGENTLY discussed with the Health Security Agency (HSA) in the UK, previously known as Public Health England, as well as the High Security Infectious Diseases Unit at the Royal Free Hospital London and the Imported Fever Service at Porton Down. This is for a surveillance activity rather than “infection severity” at the moment but as we all know, new infections that can spread can become a problem!
Treatment
There is no specific treatment for Monkey Pox, and most cases are mild and self-limiting. In severe cases the drug Cidofovir has been used. Cidofovir is a nucleoside analogue drug; it mimics a component of the virus’s genetics which when incorporated into the new virus particle causes a fault and the virus can’t reproduce. The main problems with Cidofovir are that it is only available intravenously and it is very toxic to kidneys.
There are now 2 new experimental drugs for treating pox-illnesses like Monkey Pox (and even Smallpox!) that might be available for very unwell patients in an off-license capacity:
- Brincidofovir is a derivative of Cidofovir which is orally bioavailable and is less toxic to kidneys
- Tecovirimat is a novel drug that is also orally bioavailable but works by preventing newly reproduced virus from wrapping up into a small package prior to release – there is experimental evidence that Tecovirimat and Brincidofovir are synergistic with each other (the combined effect is greater than either on its own)
Prevention
The main methods of prevention are avoidance of exposure to infected animals and people, good infection control practice and vaccination (the Smallpox vaccine is 85% effective at preventing Monkey Pox).
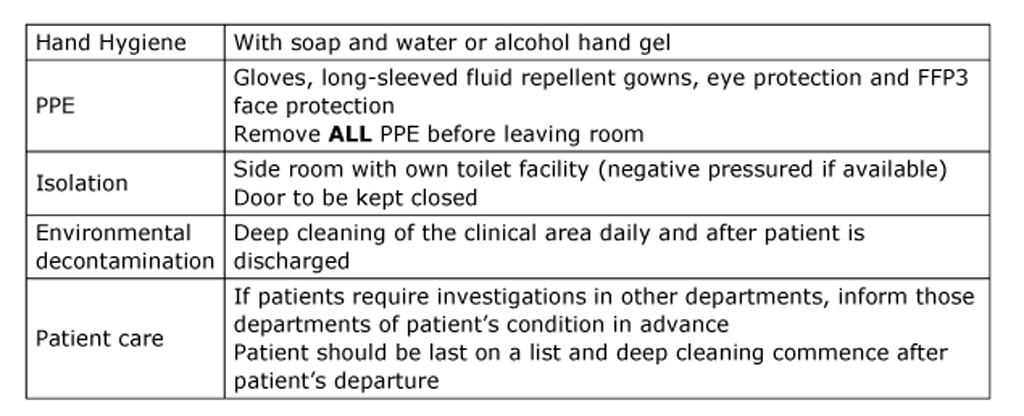
There are no definitive infection control policies for this infection yet, but in the meantime the following for respiratory spread infections would be appropriate:
Now we wait to see what happens. Will there be further cases? Will the virus become established in the MSM population? If it does we could be in for another viral “pandemic”… oh joy!
Oops since writing this on Tuesday we now have 20 cases in the UK… did I say watch this space?!

 RSS Feed
RSS Feed
