Basic Bacterial Identification by Microscopy
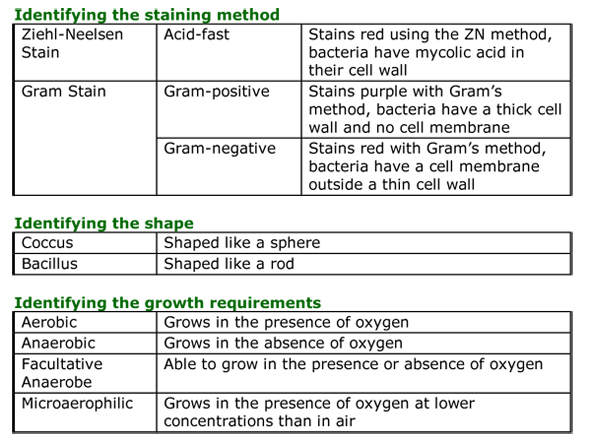
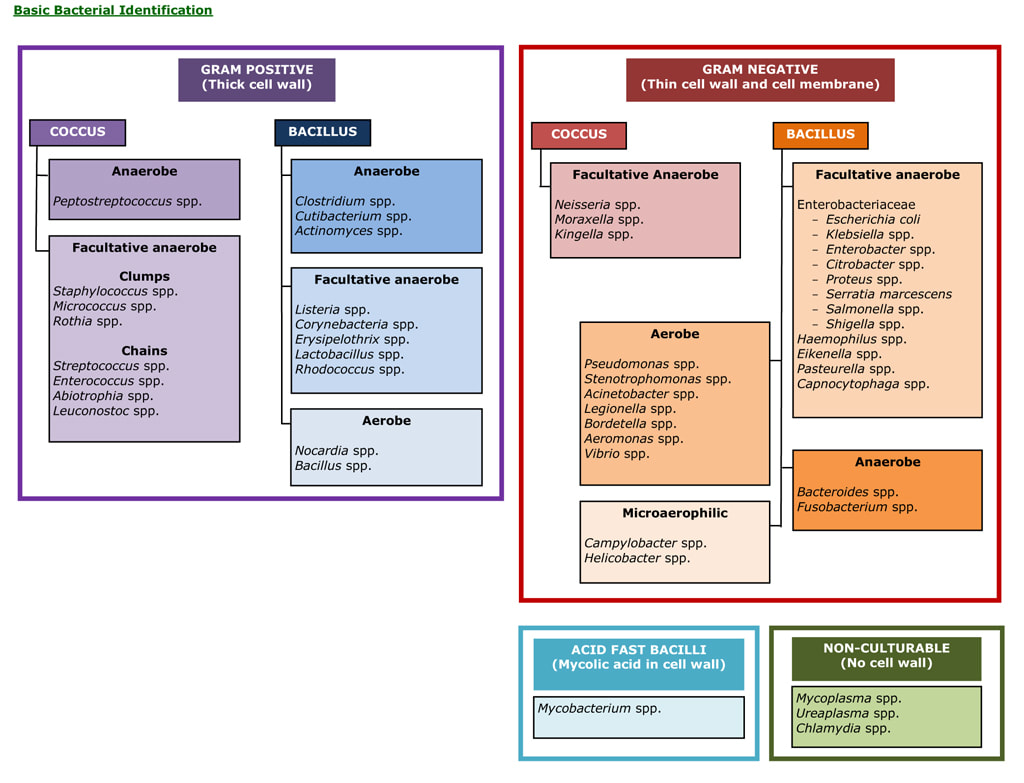
There are too many microorganisms to remember therefore they need to be separated into groups with similar features. Microbiologists use a number of terms to describe the different appearances of bacteria; Gram-positive or Gram-negative, coccus or bacillus etc. For example, the Microbiologist might telephone with a result, saying “the cause is a Gram-negative bacillus growing both aerobically and anaerobically”. This may appear to be pointless jargon but using a simple system of firstly identifying the staining method, then the shape of the microorganism and finally the microorganisms growth requirements, a doctor can begin to eliminate microorganisms, like in a game of Cluedo, in order to identify the most likely cause of the infection.
If a microorganism is Gram-negative, it cannot be any of the Gram-positives or acid-fast bacilli and therefore these can be discarded. If the microorganism is bacillus shaped then all of the cocci can be discarded. If the microorganism is then described as growing anaerobically, the aerobes can be discarded; and if it is also described as growing aerobically as well as anaerobically the anaerobes can also be discarded. This identifies the microorganism as a Gram-negative bacillus growing as a facultative anaerobe i.e. an Enterobacteriaceae, Haemophilus spp., Eikenella spp., Pasteurella sp. or Capnocytophagus spp. The clinical history can then narrow the list further because if the patient has CAP it is probably a Haemophilus sp., if they have a cat bite it is probably Pasteurella sp., and if they have pyelonephritis it will be one of the Enterobacteriaceae.
If a microorganism is Gram-negative, it cannot be any of the Gram-positives or acid-fast bacilli and therefore these can be discarded. If the microorganism is bacillus shaped then all of the cocci can be discarded. If the microorganism is then described as growing anaerobically, the aerobes can be discarded; and if it is also described as growing aerobically as well as anaerobically the anaerobes can also be discarded. This identifies the microorganism as a Gram-negative bacillus growing as a facultative anaerobe i.e. an Enterobacteriaceae, Haemophilus spp., Eikenella spp., Pasteurella sp. or Capnocytophagus spp. The clinical history can then narrow the list further because if the patient has CAP it is probably a Haemophilus sp., if they have a cat bite it is probably Pasteurella sp., and if they have pyelonephritis it will be one of the Enterobacteriaceae.
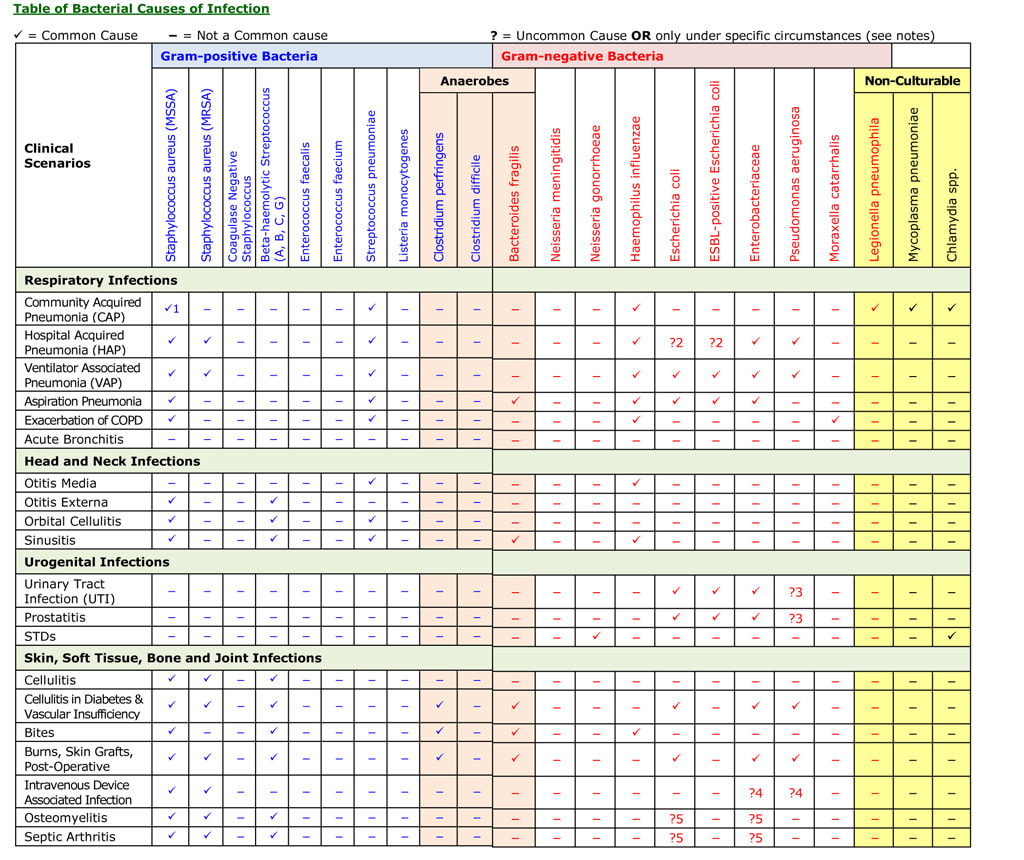
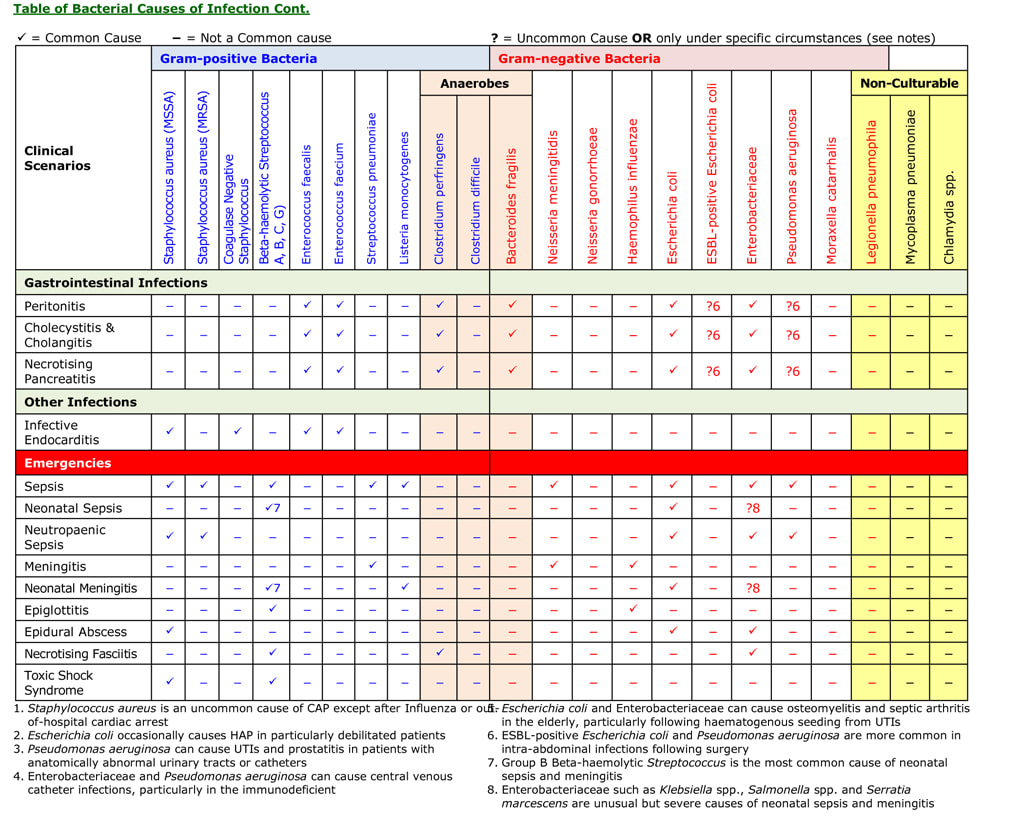
Knowledge of bacterial identification from the Gram film appearance helps predict the cause of an infection from the microscopy result up to 48 hours before the culture result is available. By using both the Basic Bacteria Identification diagrams and the Table of Bacterial Causes of Infection (following diagrams) you can identify the likely bacteria from the Gram film appearance on the microscopy result. For example:
• The patient clinically has meningitis; the Gram film of the CSF shows Gram-positive cocci in chains. Meningitis is caused by Streptococcus pneumoniae, Listeria monocytogenes, Neisseria meningitidis, Haemophilus influenzae and Mycobacterium tuberculosis. We know it is Gram-positive therefore ruling out Neisseria meningitidis, Haemophilus influenzae, which are Gram-negative and Mycobacterium tuberculosis, which is an acid-fast bacillus. The microscopy also states coccus, which rules out Listeria monocytogenes as this is a bacillus. This leaves Streptococcus pneumoniae, a chain forming Gram-positive coccus.
• The patient clinically has septic arthritis; the Gram film of the synovial fluid shows Gram-positive cocci in clumps. Septic arthritis is caused by Staphylococcus aureus, Beta-haemolytic Streptococcus, Escherichia coli and Enterobacteriaceae. As it is Gram-positive this rules out Escherichia coli and Enterobacteriaceae, which are Gram-negative. The microscopy also states clumps, which rules out Streptococcus sp. as these form chains. This leaves Staphylococcus aureus, a clump forming Gram-positive coccus.
• The patient clinically has peritonitis; the Gram film of the peritoneal fluid shows Gram-positive cocci in chains, Gram-positive bacilli and Gram-negative bacilli. Peritonitis is caused by bowel flora including: Enterococcus sp., Clostridium sp., Bacteroides sp., Escherichia coli and Enterobacteriaceae. The mixed Gram film appearance shows the presence of the entire bowel flora. This indicates the patient has probably perforated their bowel rather than developed spontaneous bacterial peritonitis. Even this result is helpful as it indicates there is a hole in the bowel. The patient needs surgery not just antibiotics, as no antibiotic tablet is large enough to plug the hole! Antibiotics will only help if the hole is surgically repaired.
• The patient clinically has meningitis; the Gram film of the CSF shows Gram-positive cocci in chains. Meningitis is caused by Streptococcus pneumoniae, Listeria monocytogenes, Neisseria meningitidis, Haemophilus influenzae and Mycobacterium tuberculosis. We know it is Gram-positive therefore ruling out Neisseria meningitidis, Haemophilus influenzae, which are Gram-negative and Mycobacterium tuberculosis, which is an acid-fast bacillus. The microscopy also states coccus, which rules out Listeria monocytogenes as this is a bacillus. This leaves Streptococcus pneumoniae, a chain forming Gram-positive coccus.
• The patient clinically has septic arthritis; the Gram film of the synovial fluid shows Gram-positive cocci in clumps. Septic arthritis is caused by Staphylococcus aureus, Beta-haemolytic Streptococcus, Escherichia coli and Enterobacteriaceae. As it is Gram-positive this rules out Escherichia coli and Enterobacteriaceae, which are Gram-negative. The microscopy also states clumps, which rules out Streptococcus sp. as these form chains. This leaves Staphylococcus aureus, a clump forming Gram-positive coccus.
• The patient clinically has peritonitis; the Gram film of the peritoneal fluid shows Gram-positive cocci in chains, Gram-positive bacilli and Gram-negative bacilli. Peritonitis is caused by bowel flora including: Enterococcus sp., Clostridium sp., Bacteroides sp., Escherichia coli and Enterobacteriaceae. The mixed Gram film appearance shows the presence of the entire bowel flora. This indicates the patient has probably perforated their bowel rather than developed spontaneous bacterial peritonitis. Even this result is helpful as it indicates there is a hole in the bowel. The patient needs surgery not just antibiotics, as no antibiotic tablet is large enough to plug the hole! Antibiotics will only help if the hole is surgically repaired.
Topics in Microbiology:
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).
- How to Take Microbiology Specimens
- Why Bother Completing Request Forms?
- What is Relevant Information for a Request Form?
- Considerations When Contacting a Microbiologist for Advice
- A to Z of Microbiology Tests by Microorganism or Condition
- A to Z of Microbiology Tests by Specimen Type
- Microbiology Results (by Specimen Type)
- How to Interpret Microbiology Results - Bacteriology
- Examples of Bacteriology Requests, Results and Interpretations
- Why Can’t I Do Every Test?
- Examples of Pre and Post-test Probability Results and Interpretations
- How to Use Pre-test Probability, Likelihood Ratios and Post-test Probabilities in the Clinical Setting
- Basic Bacterial Identification by Microscopy
- Basic Bacterial Identification
- Table of Bacterial Causes of Infection
- How to Interpret Microbiology Results – Serology and Virology
- Examples of Serology / Virology Requests, Results and Interpretations
- Notifiable Infectious Diseases in the UK
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).