Meticillin Resistant Staphylococcus aureus (MRSA)
MRSA is Staphylococcus aureus that has acquired resistance to the antibiotic Meticillin. REMEMBER MRSA is resistant to all of the Beta-lactam antibiotics in common use: Flucloxacillin, Co-amoxiclav, Piptazobactam, Cephalosporins and Carbapenems. Although hospitals and the Department of Health concentrate on MRSA figures, 3% of the population carry MRSA as part of the normal flora in their nose and 30% of the population carry Meticillin sensitive Staphylococcus aureus (MSSA) as part of their normal flora.
Mode of Transmission
Incubation Period
Period of Communicability
Screening
Current UK practice is to screen all previously positive patients and all new patients admitted to high-risk units including:
Body sites to screen include:
Suppression Therapy
All Cases
Nasal ointment:
Mupirocin 2% (BactrobanR) applied to inside of the nose 3x/day for 5 days
Alternative NaseptinR (Chlorhexidine PLUS Neomycin) 4x/day for 10 days
PLUS for Adults
Body and hair wash:
4% Chlorhexidine 1x/day for 5 days (alternative Octenisan wash 1x/day for 5 days)
Patients should be re-screened 48 hours after MRSA suppression therapy has stopped. If the patient remains positive continue to manage as MRSA positive. If the patient tests negative, rescreen at 48 hourly intervals until 3 negative screens at which point the patient is considered MRSA-free. If any of these screens are positive then continue to manage the patient as MRSA positive.
Mode of Transmission
- MRSA is usually transmitted between patients on the hands of healthcare staff or on contaminated equipment (fomites).
Incubation Period
- MRSA are able to colonise people. Once the microorganism is part of the patient’s normal flora it can potentially cause infection and be spread to others at any time. The majority of infections with MRSA follow previous colonisation.
Period of Communicability
- Potential cross infection can occur at anytime whilst the patient remains colonised with the resistant bacteria, however risk is highest when patients have skin diseases that allow heavy shedding of bacteria e.g. eczema, psoriasis.
Screening
Current UK practice is to screen all previously positive patients and all new patients admitted to high-risk units including:
- Vascular surgery
- Neurosurgery
- Cardiothoracic surgery
- Orthopaedics and trauma
- Critical care (ICU, HDU, SCBU)
- Renal dialysis
- Haematology and oncology
- Coronary Care
Body sites to screen include:
- Nose
- Groin
- Umbilicus in neonates
- Wounds – any breach in skin including IV catheter sites (separate swab for each site or you risk transmitting bacteria)
- Urine if patient catheterised
- Sputum if productive cough
Suppression Therapy
All Cases
Nasal ointment:
Mupirocin 2% (BactrobanR) applied to inside of the nose 3x/day for 5 days
Alternative NaseptinR (Chlorhexidine PLUS Neomycin) 4x/day for 10 days
PLUS for Adults
Body and hair wash:
4% Chlorhexidine 1x/day for 5 days (alternative Octenisan wash 1x/day for 5 days)
Patients should be re-screened 48 hours after MRSA suppression therapy has stopped. If the patient remains positive continue to manage as MRSA positive. If the patient tests negative, rescreen at 48 hourly intervals until 3 negative screens at which point the patient is considered MRSA-free. If any of these screens are positive then continue to manage the patient as MRSA positive.
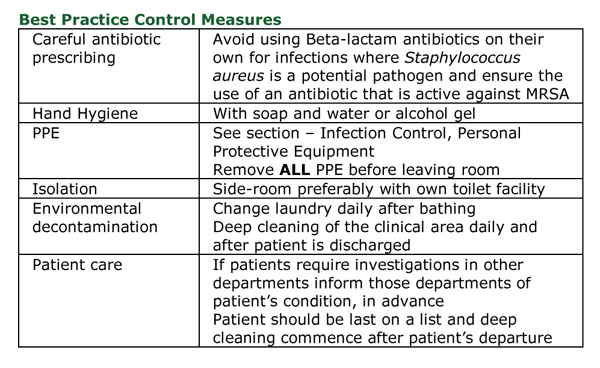
Topics in Infection Control:
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).
- What is Infection Control?
- Root Cause Analysis (RCA)
- Example of the RCA Process - A patient gets CDAD
- Universal Precautions and Hand Hygiene
- Personal Protective Equipment (PPE)
- Summary of Isolation Priority and Infection Control Precautions
- Influenza
- Tuberculosis (TB)
- Multidrug Resistant Tuberculosis (MDR TB)
- Respiratory Spread Viral and Bacterial Infections
- Clostridium difficile Associated Disease (CDAD)
- How Clostridium difficile can Spread in a Ward Environment
- Diarrhoea and Vomiting (D&V)
- Multiple Antibiotic Resistant Gram-negative Bacteria
- New Antibiotics for Treating Resistant Gram-negative Bacteria
- Meticillin Resistant Staphylococcus aureus (MRSA)
- Panton-Valentine Leukocidin (PVL) Positive Staphylococcus aureus
- Glycopeptide Resistant Enterococcus (GRE)
- Viral Haemorrhagic Fever (VHF)
- Needlestick Injuries
- Needlestick Injury HIV PEP Flowchart
- Outbreaks
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).