Clostridium difficile Associated Disease (CDAD)
Clostridium difficile Associated Disease (CDAD) is the most common cause of antibiotic associated diarrhoea. Symptoms usually present 5-10 days after starting antibiotics. Up to 3% of the general population are asymptomatic carriers of Clostridium difficile and although they do not have symptoms they represent a potential infection control issue as they can spread the infection.
Diagnosis of CDAD
• One or more episodes of stool loose enough to take the shape of the container (types 5-7 on the Bristol Stool Chart, see Appendix 2)
- PLUS not attributable to another cause including medicines
- PLUS a positive laboratory test for Clostridium difficile toxin
• OR evidence of pseudomembranous colitis on endoscopy
Diagnosis of CDAD
• One or more episodes of stool loose enough to take the shape of the container (types 5-7 on the Bristol Stool Chart, see Appendix 2)
- PLUS not attributable to another cause including medicines
- PLUS a positive laboratory test for Clostridium difficile toxin
• OR evidence of pseudomembranous colitis on endoscopy
|
Risk Factors for Severe Disease:
|
|
Clinical Features
• Diarrhoea
• Nausea
• Dehydration
• Abdominal pain
• Fever
• Bowel perforation
• Toxic megacolon (>6cm diameter with no obstruction)
• Nausea
• Dehydration
• Abdominal pain
• Fever
• Bowel perforation
• Toxic megacolon (>6cm diameter with no obstruction)
Causes
CDAD is caused by a toxin produced by the bacterium Clostridium difficile.
Investigations
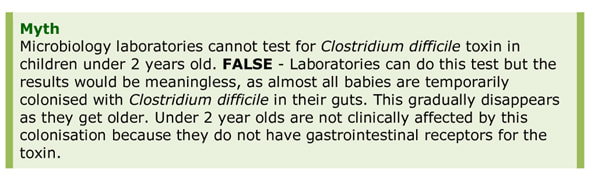
- Stool (liquid stool only) 2-stage test taking 3-4 hours and performed daily by laboratories
- All outpatients >65 years old, with a liquid stool sample
- Outpatients under 65 years old, with a liquid stool sample, if specifically requested
- Sampling to test for cure is not required; 50% of successfully treated patients have positive tests up to 6 weeks after infection has cleared
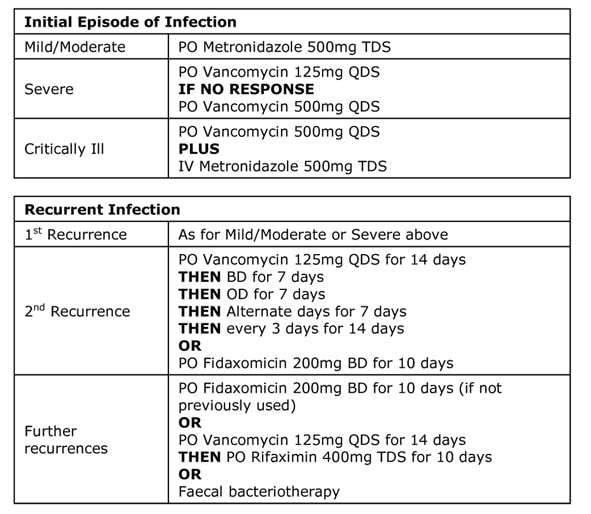
Treatment
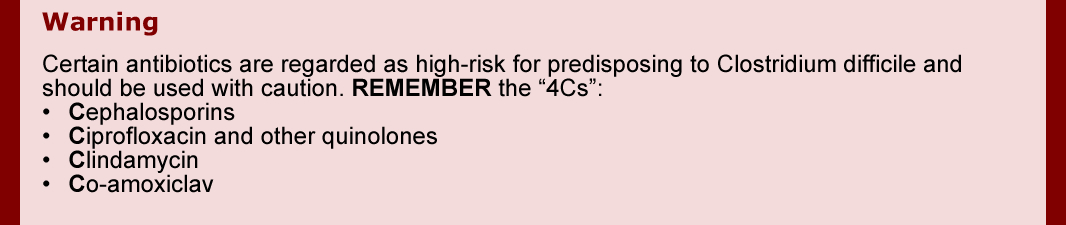
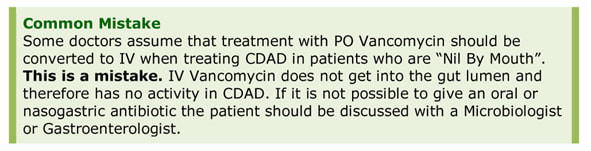
Stop the offending antibiotic. If the patient still requires treatment for another infection then discuss the options with a Microbiologist and consider continuing Clostridium difficile treatment for 1 week beyond stopping the other antibiotics. Severe and critically ill patients need an urgent surgical review.
|
Antibiotics that DO NOT normally predispose to CDAD: |
|
Faecal Bacteriotherapy
Faecal bacteriotherapy, also known as “faecal transplantation”, involves replacement of the colonic contents with stool containing normal flora from a donor. Donors are screened for various infections prior to donation; samples are held frozen in a “faeces donor bank” up until they are required. Faecal bacteriotherapy has a 94% cure rate in pseudomembranous colitis caused by Clostridium difficile. The lack of widespread adoption in the NHS, even though it is approved by the National Institute for Health and Care Excellence (NICE), is related to the social and medical stigmatisation associated with the concept of deliberately introducing someone else’s faeces into another person.
Total Duration
Initial Episode: 14 days
Recurrent Infections: as stated in treatment table
Dosing
See section - Antibiotics, Empirical Antibiotic Guidelines.
Prognosis and Complications
90% of patients with CDAD respond to treatment. However, 20-30% of these have recurrent infection. These patients should be retreated or offered faecal bacteriotherapy which has a 94% cure rate in pseudomembranous colitis. The mortality from toxic megacolon is 64%.
Prophylaxis and Prevention
Clostridium difficile can exist as both spores and vegetative bacteria and therefore can survive drying. The bacteria can persist in the environment for a long time and hence the need for deep cleaning between patients. Environmental control is the best way to prevent CDAD.
Infection Control Precautions
See section – Infection Control, Clostridium difficile Associated Disease.
Initial Episode: 14 days
Recurrent Infections: as stated in treatment table
Dosing
See section - Antibiotics, Empirical Antibiotic Guidelines.
Prognosis and Complications
90% of patients with CDAD respond to treatment. However, 20-30% of these have recurrent infection. These patients should be retreated or offered faecal bacteriotherapy which has a 94% cure rate in pseudomembranous colitis. The mortality from toxic megacolon is 64%.
Prophylaxis and Prevention
Clostridium difficile can exist as both spores and vegetative bacteria and therefore can survive drying. The bacteria can persist in the environment for a long time and hence the need for deep cleaning between patients. Environmental control is the best way to prevent CDAD.
Infection Control Precautions
See section – Infection Control, Clostridium difficile Associated Disease.
Topics in Clinical Scenarios - Gastrointestinal Infections:
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).
- Gastroenteritis and Diarrhoea and Vomiting (D&V)
- Clostridium difficile Associated Disease (CDAD)
- Necrotising Pancreatitis
- Cholecystitis and Cholangitis
- Peritonitis
- Viral Hepatitis
- Peptic Ulcer Disease
All these topics are covered in the book...Ready to buy your copy? Click here to buy your copy of "Microbiology Nuts & Bolts" Its updated and amazingly only slightly larger considering its got 1/3 more in it! (11cmx18cmx2.5cm).