|
Many hospitals rely heavily on aminoglycosides within their antimicrobial regimens. Locally we use Gentamicin as our go-to aminoglycoside of choice for sepsis (combined with Amoxicillin and Metronidazole) as well as for severe pyelonephritis amongst other things. In fact, it was one of my favourite choices for buying time to work out what is wrong with septic patients who cannot afford to wait for a diagnosis before treatment is started. ECIC (a.k.a. my wife) used to tease me that Gentamicin was the only Microbiology oncall advice needed and therefore our cat could do the oncall… how rude!
The Microbiologist looked around the room expectantly. The subject of today’s Registrar and Clinical Scientist teaching was zoonotic infections. In fact, it had been the subject of teaching for a number of weeks as the topic was enormous! The trainee Clinical Scientist who had suggested the topic was beginning to wonder what they had let themselves in for as the Microbiologist was clearly enjoying himself way too much!
“So, what can you tell me about deer fly fever?” he asked. The trainees all looked at the floor, the ceiling, each other, in fact anything to avoid making eye contact with their overzealous teacher. “Come on, come on” encourage the Microbiologist, “it’s a possible FRCPath exam question.” Still nothing… “Okay, what about if I said the patient had recently returned from a summer holiday in Martha’s Vineyard, a 96-square-mile island shaped like a shark’s tooth off the coast of Massachusetts, with a high fever and severe pneumonia?” The silence was deafening… Then the Registrar piped up “isn’t that where the 2010 film Ghost Writer was set? Yeah, Martha’s Vineyard, yep, I’m sure it was! Some big cast names in it too”. No, I’m serious… what is Covid? I hear it all the time. Someone coughs, is it Covid? Someone sneezes, is it Covid? Some say they feel a bit under the weather, is it Covid? I even had the discussion with my parents at the weekend… ECIC (aka my wife) has a bit of a cold and they say, “has she got Covid?”
So, what is Covid? To start with, “Covid” isn’t anything. The actual name for the disease cause by the Severe Acute Respiratory Coronavirus type 2 (SARS CoV2) was Covid-19; it was an acronym for COronaVirus Infectious Disease 2019. But now it has been reduced to a snappier “Covid”. I have also been asked if someone has “caught covid”…NO! You cannot catch Covid-19, you can catch SARS CoV2, that is the name of the virus. It is so reminiscent of the horror show that was HIV back in the 1980s… even senior health professionals thought you could catch AIDS (Acquired Immune Deficiency Syndrome) …NO! You cannot catch AIDS, you can catch Human Immunodeficiency Virus (HIV). Covid-19 and AIDS are the names of the clinical diseases, not the causative viruses. So, when we think about Covid-19 being a disease, a group of symptoms if you like, then the question “what is Covid-19?” actually starts to make more sense. Back in 2018 I wrote a blog called “Don’t monkey around with the pox”. The subject was a disease called Monkey Pox, and I wrote it because the UK had recently diagnosed the first 2 cases ever in the UK. The patients were both from Nigeria. Monkey Pox is a rare infection though, and it wasn’t clear if we would see other cases again… until now…! At the beginning of May this year a new case of Monkey Pox was diagnosed in a patient who had recently come to the UK from Nigeria. Then towards the middle of May 2 further cases of Monkey Pox were diagnosed in the same household, but these patients had no contact with the first case, or any travel history, and in fact it’s not clear where they acquired their infections from. All very worrying… Then a further 4 cases have been diagnosed! Also unrelated to the previous cases and with no obvious source for the infection… however these cases have all occurred in gay or bisexual men who have sex with men (MSM). This is extremely concerning! We have now had 6 cases of Monkey Pox in people who have not been to Africa and who have no obvious source for the infection. This means we have an unknown source of infection in the UK population. On top of this we now have cases in a group of the population where spread may occur more readily through sexual activity. It is very unlikely that these 7 cases are going to be the last cases identified! So, time for an update… what has changed since the blog in 2018? Epidemiology Monkey Pox is still a rare infection. In the Democratic Republic of the Congo where most cases have been reported, surveillance studies during “outbreaks” have shown an incidence of past infection between 0.001-0.05% of the population, that’s about 1 in 100,000, but that’s when they are looking for cases during an outbreak, not all the time, so the true rate could be lower than this. There are 2 main types of Monkey Pox, West African and Central African. West African causes a milder infection with a mortality of about 1%; Central African is more severe with a mortality of about 10%. Fortunately for us, the cases in the UK so far have all been the West African type and are therefore mild infections. Person-to-person transmission is rare, with a household secondary case rate of 8%, but transmission can still occur from touching infective lesions, respiratory droplets and possibly also sexual contact. Case definition The current UK case definition for a probable case of Monkey Pox is:
The rash of Monkey Pox is vesicular (small fluid filled blisters) starting 1-5 days after onset of fever. It usually starts on the face or genitalia and then spreads to the rest of the body. It may look similar to chicken pox. Skin lesions eventually scab over, dry and then fall off. Any patient meeting the case definition should be URGENTLY discussed with the Health Security Agency (HSA) in the UK, previously known as Public Health England, as well as the High Security Infectious Diseases Unit at the Royal Free Hospital London and the Imported Fever Service at Porton Down. This is for a surveillance activity rather than “infection severity” at the moment but as we all know, new infections that can spread can become a problem! Treatment There is no specific treatment for Monkey Pox, and most cases are mild and self-limiting. In severe cases the drug Cidofovir has been used. Cidofovir is a nucleoside analogue drug; it mimics a component of the virus’s genetics which when incorporated into the new virus particle causes a fault and the virus can’t reproduce. The main problems with Cidofovir are that it is only available intravenously and it is very toxic to kidneys. There are now 2 new experimental drugs for treating pox-illnesses like Monkey Pox (and even Smallpox!) that might be available for very unwell patients in an off-license capacity:
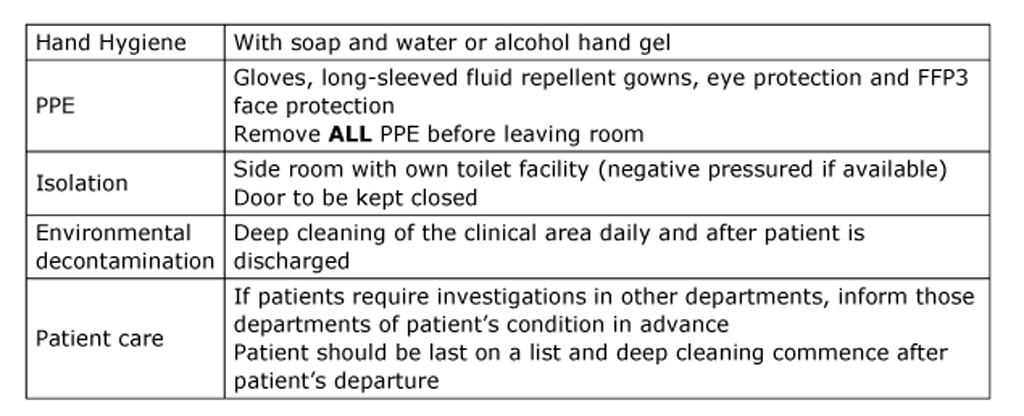
Prevention The main methods of prevention are avoidance of exposure to infected animals and people, good infection control practice and vaccination (the Smallpox vaccine is 85% effective at preventing Monkey Pox). There are no definitive infection control policies for this infection yet, but in the meantime the following for respiratory spread infections would be appropriate: In the event of a sustained outbreak in the UK it is possible that the HSA might start to ring vaccinate at risk people (e.g. MSM population) to prevent spread of the virus within the wider population.
Now we wait to see what happens. Will there be further cases? Will the virus become established in the MSM population? If it does we could be in for another viral “pandemic”… oh joy! Oops since writing this on Tuesday we now have 20 cases in the UK… did I say watch this space?! Doctors love acronyms; they use them all the time. They’re bad enough when they’re talking:
“Urine bugs may be a sign of aggressive prostate cancer”, that was the headline on the BBC news and so I had to take a look. The BBC reports that “scientists have identified urine bacteria which are linked to aggressive prostate cancer” and that “clearing the infection might prevent bad tumours”; the researchers claim they have demonstrated “an association between the presence of bacteria in urine sediments and higher D’Amico risk prostate cancer patients” and that “specific anaerobic bacteria genera have prognostic potential”
How do you predict that an antibiotic is going to be able to treat an infection caused by a particular bacterium? Easy… you do the antibiotic sensitivities and if it is susceptible you treat. Right?
Well, sometimes it isn’t as simple as that. Sometimes you need more than just a standard laboratory investigation… you need to take your antibiotic testing to another level… do you mean levitation?! I can just imagine the conversation:
“Goldberger, I need you to go down South and investigate an outbreak” demanded the Surgeon General. “Yes Sir!”, replied Dr Joseph Goldberger, “Errr, what outbreak am I investigating Sir?” “The leprosy-like skin infection outbreak that no one has ever been able to discover a cause for of course, it’s affecting millions of people down there.” “Yes Sir!” replied Dr Goldberger again, whilst probably thinking with a sinking heart “OMG, this sounds like a nightmare…” But when you work for an organisation such as the US Public Health Service in 1915 and your boss tells you to do something you pack your bags and off you go. So he did… The Microbiologist listened, getting increasingly confused. The speaker was saying that the newborn needed to drink its mother’s colostrum milk otherwise it wouldn’t have ANY antibodies. But this didn’t make sense to the Microbiologist; transfer of antibodies to the fetus via the placenta is a fundamental aspect of the immune protection a mother can give her newborn baby. We even rely on transfer by immunising in pregnancy for pertussis (whooping cough) and Covid-19 so that IgG antibody can develop in the mother, cross the placenta, and protect the baby after it has been born. It’s a FACT!
And yet, there was the speaker saying that this newborn HAD to receive its mother’s colostrum or it would have NO antibody. They even took a blood sample from the newborn to check it had antibodies AFTER it had had the colostrum. “Why are you frowning?” asked the ECIC (AKA Wife). “It doesn’t make sense” muttered the Microbiologist, “you get antibody in babies by transplacental transfer, not drinking milk.” “So, you’re saying the experts are wrong and you’re right?” “No, I’m just confused.” “Well, that’s because you’re not a vet.” Continuing to mutter under her breathe “didn’t I say I’ll marry you ONLY if you NEVER act in a medical manner towards my cats…” She had been “warned” about medical interference and the “know-it-all” attitude of medics by her vet!!! Oh, sorry, did I not say? We were watching This Farming Life (one of our favourite TV shows) and they were talking about Clydesdale foals and whether they must be given the colostrum from the mare! |
Facebook has deleted the Microbiology Nuts & Bolts pages - if you want your weekly dose of microbiology then you will need to come here, and we look forward to you continuing to read it!
Blog Author:
David Garner Please DO NOT advertise products and conferences on our website or blog
Categories
All
Archives
November 2022
Categories
All
|
| Microbiology Nuts & Bolts |
|








 RSS Feed
RSS Feed
