“This one looks interesting” he said to himself even though he knew he had been told never to use the word interesting in relation to microbiology…. Ever…!
“You have a baby boy on the ward with salmonellosis, what’s the story?” he asked when the Paediatric SHO answered the phone.
“He’s a six week old who developed bloody diarrhoea a couple of days ago and started vomiting. He was febrile and looked septic so we started him on empirical IV Ceftriaxone.”
“Any pets?” asked the Microbiologist.
“He’s only 6 weeks old, why would he have any pets?” answered the tired junior.
“Not him, the family; specifically reptiles. Any snakes or lizards?”
“I have no idea.”
“Well carry on with the IV Ceftriaxone as he has a Salmonella species in his blood culture and call me back about the reptiles… no wait, I’ll come up and ask myself.”
The junior doctor hung up. Muttering to himself about mad Microbiologists he wandered off to get on with some other work.
So why did the Microbiologist want to know about reptiles? Was he just mad or was there method to his madness?
There are 2 different genus of Salmonella; Salmonella bongori and Salmonella enterica. S. bongori is part of the normal flora of cold-blooded animals such as lizards and snakes. S. enterica is subdivided into 6 subspecies including enterica, salamae, arizonae, diarizonae, houtanae and indica. These subspecies are then further divided into approximately 2,600 serovars (serotypes) of which only a small number infect humans… don’t worry, I’m not going to list the 2,600 serovars… in fact our story features the cold-blooded varieties…
So S. bongori is a reptile gut organism and the most common time we see this is when it causes infections in herpetologists (people who keep reptiles) or, more commonly in my experience, their children! The basic problem is one of hygiene. If someone who keeps reptiles is not scrupulous with hand hygiene and keeping the environment clean they will eventually spread salmonella. Hands and clothing are major vectors for transmission; many pet owners do not realise this. Salmonella can easily be spread by the reptile keeping parent who may get their clothes and hands contaminated (this is not necessarily visible contamination! Ooh yuck reptile slime) from handling their pet if they have taken inadequate hygiene precautions before picking up their baby or playing with their child. How many pet owners think to change their clothes after handling their pet? Oh look another cat hair on my jumper!! Some pets are more contagious or “dangerous” than others. The most danger I’m in from my black cat is an evil stare when I’m late feeding her!
Some subspecies of S. enterica are also normal gut flora for reptiles, especially snakes. So, it’s not just S. bongori that we have to worry about with reptiles! In most studies, subspecies S. enterica, S. arizonae and S. diarizonae are the most common isolates; although S. houtanae and S. salamae have been documented. Curiously S. indica has not been described but I can’t find the reason for this (do you know?).
Studies looking at non-venomous snakes found carriage rates of Salmonella spp. to be as high as 81%; that’s 4 out of every 5 snakes. The rate was even higher in a collection of venomous snakes studied at the London School of Tropical Medicine, where 91% of the snakes were carriers of S. enterica subspecies. This study involved some of the World’s most venomous snakes such as the Boomslang, Saw-scaled viper and Black Mamba… but how do you study Salmonella spp. carriage in snakes?!
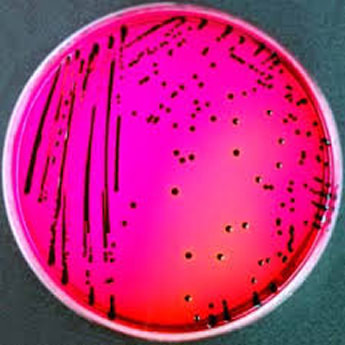
Okay, so the silly answer is “carefully”, but according to the papers on the subject it’s more sensible and far more in keeping with how us humans test for salmonella… collect a snake poo sample and then test it by normal laboratory methods such as culture on Xylose-Lysine-Desoxycholate (XLD) Agar.
XLD is both a selective and indicator agar. Desoxycholate in the agar inhibits the growth of most non-gastrointestinal bacteria but allows Salmonella spp. and Shigella spp. to grow. Xylose and Lysine are sugars used to distinguish Salmonella spp. from Shigella spp. by a pink colour change due to acid production. Salmonella spp. also produce hydrogen sulphide on XLD giving black colonies. This means the Microbiology Biomedical Scientist (BMS) can quickly screen the culture and if there are no black colonies then there is no Salmonella spp. Any black colonies need further work such as an API, MaldiTOF or PCR to confirm the identification as some other bacteria can also give black colonies on XLD (classically Proteus mirabilis and Hafnia alvei).
You would think that human salmonellosis from reptiles is rare but actually it isn’t. A number of studies have looked at this and found that 6% of all salmonella infections in the USA were from reptiles (about 76,000-140,000 cases per year); a UK study showed a whopping 27.4% of salmonellosis in under 5 year olds was from reptiles. The study also showed that the infection was more likely to involve the blood stream when the isolate was from a reptile; this may be because from an evolutionary perspective our bodies are used to “dealing with” common Salmonella spp. that cause gastrointestinal disease, whereas less common species are able to evade the gastrointestinal immune response and get into blood.
Hmmm… nearly 30% of salmonellosis in under 5 year olds was from reptiles, the study from the UK does raise the question of whether children and reptiles are a good mix?
How does salmonellosis present?
In reptiles salmonellosis is asymptomatic; they are carriers and therefore it is part of their normal flora. However in humans the most common presentation of salmonellosis is gastroenteritis with diarrhoea and vomiting within 3 days of exposure. Very occasionally Salmonella spp. can disseminate to normally sterile parts of the body such as the gallbladder, bones and joints and the urinary tract. This can cause recurrent cholecystitis, osteomyelitis, septic arthritis and pyelonephritis as well as sepsis. Infection is most severe in the very young and the very old.
How is salmonellosis treated?
Fortunately most cases of gastrointestinal salmonellosis are self-limiting and don’t require treatment. In the very young and very old, or those with disseminated infection, treatment is either IV Ceftriaxone or PO Ciprofloxacin.
How do you prevent salmonellosis from reptiles?
I found the following on the Center for Disease Control and Prevention (CDC) website and it is pretty clear advice… especially the last point!
Safe Handling Tips for Reptiles and Amphibians (CDC)
- Always wash your hands thoroughly after handling reptiles and amphibians, and anything in the area where they live or roam such as their habitats, food, or equipment.
- Children younger than 5, people with weak immune systems, and adults older than 65 should not handle or touch amphibians, reptiles or their environment. These groups have a higher chance of serious illness and hospitalisation from Salmonella germs.
- Don’t cross-contaminate! You don’t have to touch a reptile or amphibian to get sick from their germs. Any reptile food such as frozen or live rodents, equipment, and materials, including the water, can be contaminated with Salmonella and other germs.
- Keep your reptiles and amphibians and their equipment out of your kitchen or anywhere human food is prepared, served, or eaten.
- Clean reptile and amphibian habitats outside your home using warm, soapy water. If you cannot clean items outside of your home, clean items in a dedicated bin/tub; remember to also clean the bin/tub and any surfaces it touches.
- Don’t kiss or snuggle with reptiles and amphibians.
Who the heck kisses or snuggles a snake… okay you might if you really love your snake…. But really!?
The Microbiologist wandered up to the ward, grateful for the excuse to get away from the Duty desk for a while. He introduced himself to the little boy’s parents and asked what reptile they had. They looked at the Microbiologist in amazement. How did he know they have a bearded dragon called “George”?
So the little boy was treated with IV Ceftriaxone for 10 days until he was back to normal. His parents felt terrible that they had allowed their son to become infected with Salmonella and before their son had left the hospital the families pet bearded dragon had been rehomed with a friend who was also an amateur herpetologist and who’s children had all grown up and left home… but I suspect George will be moving back in when the little boy is a bit older… ah well, best all round really. I have to admit I have a bit of a soft spot for reptiles myself… but I prefer seeing wild ones and certainly wouldn’t kiss and snuggle one!


 RSS Feed
RSS Feed
