The patient presented to the hospital with a high fever, headache and conjunctivitis. The medical team called me (the microbiologist) concerned that this patient might be developing some odd form of meningitis because of his headache. The patient clearly looked “sporty” and on detailed questioning it turned out that a few days earlier he had been rowing on the River Thames and had decided to jump into the water to cool down. The evening before the patient presented to the hospital he began to get sore, red eyes, which streamed a lot but had no purulent discharge. He then developed a fever of 39°C, muscle pains in the legs and hips, and a headache. By the time I saw him he had developed a widespread rash.
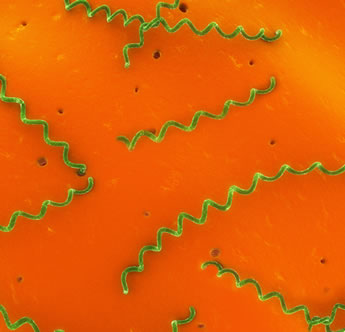
Bloods were taken to look for antibodies against the bacteria Leptospirosis icterohaemorrhagica and the patient was started on IV Benzylpenicillin. Two hours later the patient developed fever, chills, rigors, hypotension, tachycardia, vasodilation and myalgia and hyperventilation. However the team had been warned to observe the patient carefully in order to recognise this response, Jarisch Herxheimer reaction (a severe allergic response, usually within the first 24hours of giving the antibiotic, caused by the antibiotic rapidly destroying the bacteria causing the release of endotoxins). The team quickly acted treating with anti-inflammatory drugs, steroids and fluids to maintain blood pressure, reversing this potentially life-threatening side-effect. If the team had treated for meningitis, the diagnosis would have been missed and the extreme response to treatment may not have been at the forefront of medical team’s minds. Even though the antibiotic Benzylpenicillin can have this potentially serious side-effect, it is still the treatment of choice for severe Leptospirosis.
Two days later, when the patient was feeling much better he was switched to PO Doxycycline and allowed to go home. After one week of Doxycycline the patient made a full recovery. The serology results confirmed that the patient had Leptospirosis. The correct diagnosis and treatment ensured the patient did not stay in hospital longer than required, a diagnosis of meningitis would have required 7-21 days IV antibiotics (depending on causative micro-organism).
 RSS Feed
RSS Feed
