The Microbiologist knew that the best antibiotic for the infection was a penicillin, Flucloxacillin, so decided to try and get to the bottom of the penicillin allergy story. Side effects from antibiotics are common (e.g. diarrhoea and vomiting) but do not usually represent allergy. They sat down with the patient and asked them to describe what happened when they were last given a penicillin.
Up to 20% of patients say they are allergic to penicillin; the actual rate is only 5%. On closer questioning what patients are describing are either side effects or a symptom unrelated to the antibiotic. These side effects do not necessarily prevent the use of antibiotics in future episodes of infection.
Only 10-20% of patients who say they are allergic to penicillin are actually allergic to penicillin. This means that for the other 80-90% of patients the choice of antibiotic for treating their current infection is being unnecessarily restricted based on incorrect information.
In the era of increasing antibiotic resistance this can be a potentially life threatening error. For example, if someone is septic with a multiple-antibiotic resistant Gram-negative bacteria which is only sensitive to carbapenems, Amikacin and Colistin, reporting a severe allergy to penicillin might mean they get Amikacin or Colistin for their infection rather than the safer Meropenem. If they go in to renal failure as a result of these antibiotics or have an infection in a site where these antibiotics don’t penetrate (e.g. an abscess) then they might die. It is both the infection and the “penicillin allergy” that will have killed them. This may seem a little melodramatic but I come across the scenario where patients are treated with a less effective antibiotic because of penicillin allergy on a daily basis, even if most of the time this doesn’t lead to long-term harm, there is plenty of evidence that penicillin allergy leads to increased length of hospital stay, poorer outcomes and complications e.g. Clostridium difficile due to fluoroquinolone use.
What is penicillin allergy?
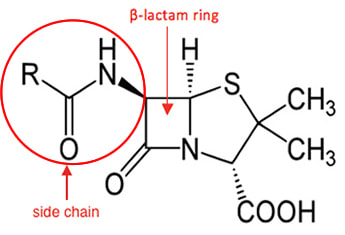
Penicillin allergy and beta-lactam allergy are often used to describe the same allergic reactions but they are actually different. Penicillin allergy strictly speaking is an allergy to a penicillin drug e.g. Benzylpenicillin, Amoxicillin, Flucloxacillin, Temocillin, Co-amoxiclav, Piptazobactam etc. Beta-lactam allergy, on the other hand, is an allergy to any antibiotic which has a beta-lactam ring or similar structure e.g. penicillins, cephalosporins, carbapenems. True beta-lactam allergy is uncommon, only about 15% of “penicillin allergy” is actually an allergy to the beta-lactam ring, see picture below.
Looking at the risk of cross reactions from a statistical point of view gives the following risk of cross reacting between types of antibiotics.
The most important risk factor for penicillin allergy is previous exposure to penicillin. The greater the exposure the higher the risks e.g. cystic fibrosis patients or those with severe chronic obstructive pulmonary disease often receive multiple courses of antibiotics which means over time they develop allergies to these antibiotics. Older age and female gender are also more often associated with penicillin allergy but this might be explained by the association with more antibiotic use in these two groups.
It is also important to remember that a patient without any previous history of penicillin allergy can still react to penicillin; it might be the first time they have reacted so make sure it is documented clearly and the patient is fully informed about what happened.
There is no 100% safe method for excluding penicillin allergy but the risks can be reduced with careful history taking about the reported reaction to the penicillin.
Taking a penicillin allergy history
- What was the name of the antibiotic they were given? – if necessary suggest examples e.g. Amoxicillin, Augmentin, Cefalexin
- Why was the antibiotic given? – Amoxicillin can cause a rash if given in glandular fever but this is not an allergy but in fact an autoimmune reaction between the antibiotic and EBV related antibodies
- How long ago was this reaction? How old where they? – there is evidence1 that if a patient hasn’t been given a penicillin for more than 15 years their body will have “forgotten” the allergy and they will no longer be allergic
- Have they ever been given an antibiotic whose name began with “ceph”? What happened? – cross reactivity between penicillins and cephalosporins occurs in only about 5% of patients therefore if a patient has been given a cephalosporin safely in the past then they are unlikely to be allergic to the beta-lactam ring and it is likely to be safe for them to have the same type of antibiotic again
- Did the reaction happen immediately or within 60 minutes? – IgE mediated reactions occur quickly and include anaphylaxis, rashes and urticaria, and these reactions are of major concern (see contraindications to penicillins below)
- What was the reaction; rash, shortness of breath, facial swelling, shock, diarrhoea, vomiting? – reactions occurring after 60 minutes are usually mediated by cytokines from T cells and include maculopapular or urticarial rashes, as well as the less common but more severe Stevens-Johnson syndrome, toxic epidermal necrolysis and DRESS syndrome (in these conditions the skin reaction is severe and life-threatening with extensive sloughing of the skin appearing like a burn (see contraindications to penicillins below), diarrhoea and vomiting are side-effects and not allergic reactions
- Where they admitted to hospital with the allergic reaction? – this helps describe the severity of the reaction as patients with severe reactions are likely to be admitted to hospital
If further evaluation of the allergy is required then allergy testing (skin testing and drug provocation testing) by an Immunologist may be required. This is a specialist area and there aren’t many Immunologists in the UK so I’m not advocating swamping them with penicillin allergic patients. Use their services when it is essential to know whether the patient is truly allergic e.g. recurrent severe infections, an underlying clinical condition which might predispose to severe reactions or multiple-reported antibiotic allergies.
Skin testing
Skin testing involves the introduction of a small amount of the antibiotic to be tested intradermally by placing some of the antibiotic on the skin then either making a small scratch or pin prick through the skin. Different concentrations of antibiotic are used with low amounts at first just in case the reaction is severe. The skin is looked at at different times to see if there is an urticarial or erythematous skin reaction. It is important that these tests are done in a controlled environment by a specialist just in case the patient has an anaphylactic reaction.
Oral provocation testing
If the patient has a negative skin test, and has never had a late onset severe reaction, the next step is to do an oral provocation test. Slowly increasing amounts of oral antibiotic are used to test for an allergic reaction. Again these tests should only be performed by a specialist.
Contra-indications to penicillins
- A definite history of an immediate reaction (< 60 minutes) e.g. anaphylaxis, rash or urticaria
- A positive skin test
- Severe reactions which did not occur immediately (>60 minutes) e.g. Stevens-Johnson syndrome, toxic epidermal necrolysis, DRESS syndrome
So what should we do with patients who say they are allergic to penicillin?
Firstly take a detailed history of the allergy and document it in the clinical notes and on the drug chart. If the details are unclear speak to relatives or the patients GP to get more information. If the patient needs a beta-lactam antibiotic make an assessment about how important this antibiotic is against the risk of an allergic reaction e.g. life-threatening infection against the risk of a rash in which case give the antibiotic. If there is going to be a future need for multiple courses of antibiotics then consider referring the patient to an Immunologist for allergy testing.
So the patient with infective endocarditis was able to describe having penicillin over 40 years ago for a severe tonsillitis at which time they developed a white coating to their throat, difficulty swallowing due to pain, and a horrid taste in their mouth. The Microbiologist retrospectively diagnosed severe oral thrush and discussed the need to use Flucloxacillin to treat the current severe infection. The patient was pleased to learn that they weren’t actually allergic to penicillin and agreed to have Flucloxacillin. Two weeks later the patient had had no reaction to the Flucloxacillin, they had recovered from their infective endocarditis and their notes and GP record were updated with the new information.
At the end of the day, whether a patient is truly allergic or not, if they refuse to take a penicillin drug when made aware of the consequences of this decision then that is their choice. In this situation you explain to the patient that you need to prescribe a less effective treatment which may have additional side effects, document the discussion and then administer the alternative antibiotic. Explaining this to the patient is informed consent… it is their choice.
Reference
1. Natural evolution of skin test sensitivity in patients allergic to beta-lactam antibiotics. Blanca M, Torres MJ, Garcia JJ et al. J Allergy Clin Immunol 1999; 103: 918



 RSS Feed
RSS Feed
