“What makes you think they have infective endocarditis?” replied the much calmer Microbiologist.
“They have a high temperature and a prosthetic heart valve and splinter haemorrhages” responded the junior doctor, “so what antibiotics should I start?”
“Okay” said the Microbiologist, “but that's not enough to prove infective endocarditis on their own, let’s talk about Duke’s criteria…”
“But the splinter haemorrhages...surely they have infective endocarditis!?” pleaded the junior doctor.
But the Microbiologist went on and explained further…
So what is infective endocarditis (IE)?
Infective endocarditis is an infection of the endocardium of the heart, either on native heart tissue or prosthetic heart valves. IE usually implies infection of the heart valves; however infection can also be related to transmural thrombosis and congenital heart defects such as atrioseptal defects and ventriculoseptal defects. Microbiologists also often include other intra-cardiac device related infections in the diagnosis of IE e.g. pacemakers and implantable cardioverter defibrillators.
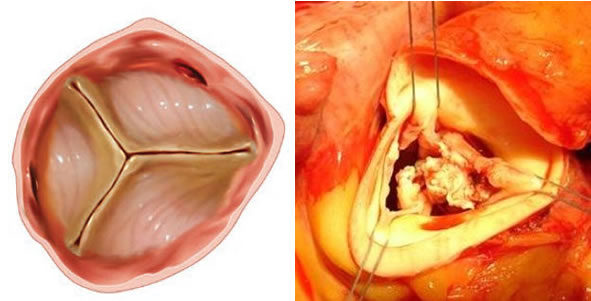
In IE an infected mass, called a vegetation, builds up on the heart tissue or valve. The vegetation is made of bacteria, fibrin and platelets and without treatment it will continue to grow until bits break off (emboli) and fly around the body or the valve itself is so badly damaged that the heart cannot function properly anymore and fails.
The diagnosis of IE is based on the Duke’s criteria, first developed in 1993 at Duke University in North Carolina in the USA. Duke’s criteria are a group of symptoms and signs that may be present in a patient with IE, the more of the criteria a patient has the more likely the diagnosis of IE. However there are some difficulties with applying Duke’s criteria in modern medicine, which I will explain later (NB: you may need to look up some of the eponymous medical jargon in Duke’s as there is way too much of it to explain it all!)
Diagnosis of infective endocarditis using Duke’s criteria requires either:
2 major criteria OR
1 major PLUS 3 minor criteria OR
5 minor criteria
Major criteria
- Typical microorganism from 2 or more sets of blood cultures, ideally more than 12 hours apart
- Positive echocardiogram showing vegetation, abscess, dehiscence of prosthetic valve or new valve regurgitation
Minor criteria
- Predisposing heart condition OR IVDU
- Fever >38°C
- Vascular phenomena – emboli, mycotic aneurysm, haemorrhages, Janeway lesions
- Immunological phenomena – glomerulonephritis, Osler’s nodes, Roth’s spots, rheumatoid factor
- Microbiological evidence – positive blood culture but falls short of major criteria (e.g. 1 set with typical microorganism, 2 or more sets with uncommon microorganism)
- Echocardiography findings – consistent with endocarditis but not a major criteria (e.g. thickened valve leaflets, transmural thrombus)
Major criteria: microbiology
So why do Duke’s criteria have the isolation of a typical microorganism from 2 or more blood cultures as one of the major criteria? In its most basic form IE is an infection in the blood stream itself and therefore the patient will have microorganisms in their blood stream all the time. This is in contrast to other infections where bacteria are in other sites and enter the blood stream intermittently; this intermittent bacteraemia is the cause of the swinging fever in patients with infections whereas in IE there is often either no fever or a low grade (37.5-38oC) continuous fever. By having two or more blood cultures separated by time you are demonstrating that microorganisms are in the blood stream continuously… i.e. intravascular infection.
The main drawback with the microbiology major criteria is when microorganisms don’t grow. The most common reason for this is that the patient has already been started on antibiotics so it is imperative that if the patient is not septic cultures are taken before antibiotics are started.
The typical microorganisms that cause IE and therefore meet Duke’s criteria are:
- Alpha-haemolytic Streptococcus sp. (also known as the Viridans streptococci)
- Streptococcus gallolyticus (previously known as Streptococcus bovis)
- Staphylococcus aureus
- Enterococcus spp.
- Streptococcus spp.
- HACEK bacteria (Gram-negative bacilli from oral flora)
When I’m advising on the investigation of a patient who may have IE my advice depends on how unwell the patient is.
- If the patient is septic and needs immediate treatment the cause is almost always Staphylococcus aureus and this grows very easily in blood cultures. In this situation I tell the team to take an immediate set of blood cultures (aerobic and anaerobic bottles) and then start antibiotics.
- If the patient is not septic I tell the doctors to hold off antibiotics and take a set of blood cultures immediately, another set in 2-3 hours and then a third set the next day (approximately 24 hours later). Taking the first 2 sets of blood cultures within 2-3 hours means that if the patient deteriorates after this time a third set can be taken and antibiotics started; this makes meeting the Duke’s major criteria more likely (2 or more blood cultures positive with a typical microorganism).
Major criteria: echocardiography
The echocardiogram evidence of IE is pretty self-explanatory. If you see a vegetation or an abscess there is clearly an infection in the heart. Likewise, dehiscence (stitching comes out) of a prosthetic valve, a new valve regurgitation showing destruction of cardiac tissue holding the prosthetic valve in place or valve regurgitation of the native valve tissue, all provide evidence of IE.
There are two main types of echocardiography, transthoracic where the ultrasound probe is placed on the outside of the chest wall, and transoesophageal where the ultrasound probe is passed into the oesophagus. There is usually less tissue in the way of an oesophageal probe and therefore the pictures are often better. As a result the sensitivity of each type is; transthoracic 60-75%, transoesophageal 95-97%... but neither is able to diagnose all cases of IE.
One of the main drawbacks to echocardiography in the modern era of medicine is actually the reason why endocarditis is becoming more common… the use of prosthetic heart valves. Prosthetic heart valves predispose to clot formation and therefore IE but they also make it harder to see what is going on in the heart with echocardiography. Valves are either metallic or tissue (porcine or bovine tissue). Even tissue valves have a ring of metallic material around the outside which is where the valve is stitched into the heart. All of this metallic tissue scatters the ultrasound signal from the echocardiogram making it virtually impossible to see what is actually going on with the valve. Because of this it is now quite uncommon to get good echocardiographic evidence of IE that meets the Duke’s major criteria.
For this reason, increasingly, the microbiology is the most important and more likely Duke’s major criteria.
Minor criteria
There are 6 minor criteria. The microbiological (1) and echocardiographic (2) minor criteria are essentially those that fall short of the major criteria e.g. only a single blood culture with a typical microorganism (i.e. unable to prove continuous bacteraemia) or echocardiography that suggests abnormal valves but the cause isn’t clear.
(3) A pre-existing cardiac condition or IVDU (IV drug use) is a risk factor for the development of IE; the IV injection of impurities with drugs causes damage to the surface of the IVDUs heart valves promoting clot formation.
(4) A fever (>38oC) indicates a possible infection.
(5) Vascular phenomena (emboli, mycotic aneurysm, haemorrhages, Janeway lesions) are evidence of infected bits of clot flying off from the vegetation and appearing somewhere else in the body. The most common emboli are known as splinter haemorrhages, small bits of necrotic skin under the nail bed where tiny clots have cut off the blood supply to the skin.
(6) Immunological phenomena like glomerulonephritis in the kidneys and Osler’s nodes usually on the hands (named after my medical hero Sir William Osler) occur due to the creation of immune complexes of antibody and antigen. These complexes get stuck in body tissues and then activate the immune system in the area causing damage to the local tissue.
Other imaging modalities in IE
There has been a lot of interest recently in the use of cardiac magnetic resonance imaging (MRI) and fluorodeoxyglucose positron emission tomography and computed tomography (FDG PET/CT) in the diagnosis of IE. Cardiac MRI may be able to detect spread of infection within cardiac tissue. In FDG PET/CT, positron-labelled glucose is taken up by active white blood cells (or other highly metabolically active cells e.g. cancer cells) which then shows where an infection might be occurring. FDG PET/CT may be able to show abscesses or spread of infection in cardiac tissue as well as complications (e.g. vascular phenomena) of IE. However, FDG PET/CT is prone to false positive results and therefore these different imaging modalities should be used with caution in the diagnosis of IE until further evaluation has taken place.
Duke’s criteria in the modern era
The vascular and immunological phenomena of IE are becoming increasingly rare in modern medicine because it usually takes a very long time for them to develop, often many months. Most patients now do not take months to present to their doctor and therefore these late features of IE are not usually present.
The rarity of vascular and immunological phenomena is another drawback to Duke’s criteria. Without these two criteria there are only 4 minor criteria left and remember, Duke’s criteria requires 5 minor criteria. Added to this if there are no major criteria (typical microbiology and positive echocardiogram), and the echocardiographic major criteria is becoming increasingly difficult to diagnose, Duke’s criteria are very difficult to fulfil. Therefore positive microbiology, that meets the Duke’s major criteria, is the ONLY real way of diagnosing IE in the modern era of medicine. At the hospital I work at the Microbiologists are now conducting a weekly cardiology MDT to help with the diagnosis of IE patients.
So having had to listen to the Microbiologist’s draft blog on using Duke’s criteria for the diagnosis of IE, the junior doctor reluctantly held off the antibiotics as the patient remained stable. The junior set off to take the recommended three sets of blood cultures over the next twenty four hours. The following day all three blood cultures were positive for a Streptococcus parasanguinis (one of the alpha-haemolytic streptococci) and the diagnosis was made; 1 major and 3 minor Duke’s criteria (temperature, prosthetic heart valve and splinter haemorrhages). The junior doctor was thrilled that their original diagnosis was indeed correct! The Microbiologist sighed in defeat, wrote up his blog and booked a table to take his wife out for a Valentine’s dinner so that she didn't end up with a broken heart. The patient was started on treatment and after four weeks of antibiotics made a full recovery.
 RSS Feed
RSS Feed
