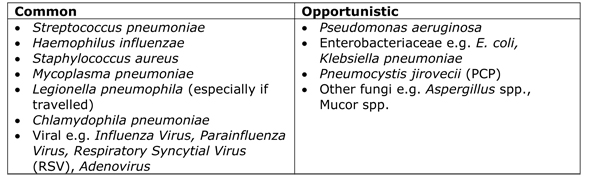
The possible cause of the patient’s pneumonia is very broad including all of the normal causes of community acquired pneumonia. However, the immunosuppression also introduces the potential of opportunistic microorganisms as well. Opportunistic infections are those caused by microorganisms which exploit the fact that the patient’s immune system doesn’t work properly but which don’t cause infection in normal patients. It is tempting to throw every treatment you can think of at this kind of patient “cos crikey they are sick”.
The normal first line treatments of severe community acquired pneumonia usually combine a beta-lactam antibiotic with a macrolide. The spectrum of activity of the beta-lactam antibiotic chosen may vary but the macrolide (where pneumonia is concerned) is consistent. The causes of pneumonia in immunosuppressed patients are:
The Amoxicillin covers:
- Streptococcus pneumoniae
- Haemophilus influenzae
The Clarithromycin covers:
- Staphylococcus aureus
- Mycoplasma pneumoniae
- Legionella pneumophila
- Chlamydophila pneumoniae
In order to cover ALL of the potential opportunistic causes of infection in an immunosuppressed patient my Registrar modified the above regimen by:
- Changing the IV Amoxicillin to IV Piptazobactam which covers the same bacteria as the Amoxicillin but ALSO COVERS Pseudomonas aeruginosa AND the enterobacteriaceae
- Adding in:
- Adding in IV Liposomal Amphotericin B for antifungal cover
Job done! A complete assortment of drugs to defend against ALL those nasty bugs! “Great stuff hey”, says my beaming Registrar the next morning. “Umm...” I say, “This all sounds great and the patient would now be on VERY broad cover for every bacteria and fungus, but what might be the consequences of this?” Looking a little glum he ponders and quickly realises he’s walking into a “mentor” trap!
Unintended consequences of prescribing
Most healthcare professionals are aware that drugs have side-effects resulting in discontinuing that treatment and switching to an alternative. The most common are nausea and diarrhoea, but others like Clostridium difficile associated disease or changes in liver function can also occur. Whilst these side-effects can be severe in their own right e.g. hepatitis, bone marrow suppression, there may be further less obvious, unintended consequences to these effects.
Let’s go back to our immunosuppressed patient with pneumonia. This patient already has two organs failing; they have bone marrow failure because of the CML and respiratory failure because of the pneumonia. If another body system fails in our patient e.g. renal failure, they would require haemodialysis but with other organs failing, due to the CML and acute pneumonia, they are unlikely to be a candidate for haemodialysis - this renal failure could trigger the end of this patients care. Multi-organ failure often results in a decision to start end-of-life care. In critically ill patients antibiotics can themselves be the reason for the organ failure, due to their side effects. In this circumstance the Registrar’s decision to cover for every possible cause of pneumonia may ultimately cause the patient’s death!
Rather than rushing in with every treatment we can think of a better approach would be to consider the likelihood of each potential cause and whether there is actually time to investigate before starting every treatment. The questions to ask yourself are “which causes are going to kill the patient quickly and what can we treat?”
The bacterial causes of pneumonia are the most likely microorganisms that will kill this patient. It is imperative that we give adequate antibacterial cover for these causes therefore the Piptazobactam and Clarithromycin are essential. The viruses might have the potential to kill the patient however there is no specific treatment to add in order to cover them (fortunately viral infections usually get better on their own and the doctor’s role is to support the patient’s organs until recovery occurs).
PCP can also kill patients quickly. If the chest X-ray is suggestive of PCP (ground glass shadowing) and the patient is profoundly hypoxic i.e. PaO2 <8kPa despite oxygen then I would also want to cover for PCP by giving Co-trimoxazole and steroids. Waiting for a diagnosis is not an option as most hospitals do not have any rapid diagnostic tests for this fungal disease.
Aspergillus spp. on the other hand rarely cause acute infections (being much slower growing microorganisms) therefore I wouldn’t initially treat for invasive aspergillosis. Sudden worsening of infection with Aspergillus spp. can occur but usually because the fungus has invaded along a blood vessel and cut off the blood supply.
Of all of the antimicrobials my Registrar considered using Amphotericin B is the most likely to cause renal failure, especially in septic patients who may well be given other nephrotoxic drugs as part of their treatment. In this situation Amphotericin B (given for the other possible fungi e.g. Aspergillus spp., Mucor spp.) is the most likely to cause another organ to fail. The resulting multi-organ failure could be the final factor leading to the initiation of end-of-life care. So in my opinion the risk of using Amphotericin B in this particular patient is not outweighed by the benefit it might bring acutely and so I wouldn’t recommend it.
I would however investigate this patient for the underlying cause. I would ask the ward doctors to send:
- Sputum cultures
- Blood cultures
- Urine for Legionella and Pneumococcal antigens
- Serum for atypical serology and Aspergillus antigens
- EDTA blood for PCP PCR (or a Bronchoalveolar lavage if the patient ends up being intubated – if not intubated the patient would be too hypoxic to tolerate this procedure)
I would then modify my treatment recommendations in the light of these results to target the specific cause and further reduce the risk of unintended consequences. If the patient was shown to have aspergillosis I would then stop everything else and start specific treatment for Aspergillus spp. such as Voriconazole which is more specific than Amphotericin B and less likely to cause renal failure. In fact this patient had a common cause of community acquired pneumonia, Streptococcus pneumoniae and treatment was narrowed down to IV Benzylpenicillin. Unfortunately despite the doctors' best efforts the patient did die. Pneumonia caused by Streptococcus pneumoniae was the actual diagnosis; which has 30% mortality in patients requiring ventilation.
So it’s important to remember that any drug, including antimicrobials, can have side-effects and the consequences of these side-effects may be more than just having to change the patients treatment. In a worst case scenario the consequences may actually be the reason the patient dies so we should always think carefully before reaching for the prescription chart.
NB The patient scenarios are always altered or completely fabricated in order to demonstrate a learning point...and in this patient story my Registrar was not actually involved...by the way my Registrar is great!
 RSS Feed
RSS Feed
