What is infection?
Infection is the presence of microorganisms causing damage to body tissues, usually in the presence of acute inflammation (pain, swelling, redness, heat and loss of function). For example Staphylococcus aureus on intact skin does not cause a problem; it is the normal flora for skin. However, if you cut your skin, Staphylococcus aureus can cause infection in the cut.
Microorganisms can also cause damage in the absence of inflammation but it is unusual, e.g. in neutropaenic patients with angio-invasive fungal infections causing tissue infarction.
Contamination is straight forward; the microorganism has been introduced into the microbiology sample from an external source e.g. poor technique when taking the sample, a swab touching a surface before being used, sneezing over a patient whilst they provide a sputum sample. Contamination can also occur when a sample is not collected correctly and the patients “normal flora” (microorganisms growing in their normal environment) gets into the sample e.g. urine taken incorrectly can contact the perineal skin and pick up from there the “normal microorganisms” which then grow in the laboratory (the presence of epithelial cells in the urine sample indicates definite contact with skin and therefore a risk of contamination… see previous, piddle in a bottle blog). Although doctors often end up treating contamination that’s not the subject of the rest of this blog… maybe another time…
What is colonisation?
Colonisation describes when bacteria grow on body sites exposed to the environment, without causing any infection. This is a normal process. These bacteria may form part of the normal flora of the individual; although colonisation is not necessarily normal flora. Occasionally, bacteria which are not normally regarded as part of the normal flora can also colonise body areas e.g. Pseudomonas spp. in a wound is not normal flora of the skin or a wound but it is not actually causing tissue damage or infection; it is just growing in the warm wet conditions of the wound. Pseudomonas spp. are the normal flora of warm wet places. Please do not treat it, when the wound is dry it will be gone! Likewise, some prosthetic devices can also become colonised with bacteria without causing infection e.g. Enterococcus spp. in urinary catheters.
When I’m deciding whether a microorganism needs treating, or not, I ask myself 3 questions:
- Is the microorganism normal flora?
- Does the microorganism cause infection at the site from where it was isolated?
- Is there inflammation or tissue destruction?
Is the microorganism normal flora?
Remember: normal flora are the microorganisms that live on another living organism (human or animal) or inanimate object without causing disease. The human body is not sterile; we become colonised by bacteria from the moment we are born. We are covered with, and contain within our intestines, approximately one hundred trillion bacteria that form the normal flora of our bodies. This normal flora helps to prevent us becoming colonised with more dangerous bacteria, which might lead to infection. We need these bugs, we should look after them and certainly not try to kill them…put down that antibacterial washing up liquid, the Dettol spray and the pocket hand sanitizer!!!
For more information about normal flora see http://www.microbiologynutsandbolts.co.uk/normal-flora.html
Does the microorganism cause infection at the site from where it was isolated?
Some bacteria are recognised pathogens of specific sites e.g. Streptococcus pneumoniae is the most common cause of pneumonia and therefore S. pneumoniae can cause infection if isolated from a sputum sample. Likewise if a microorganism is isolated from a normally sterile site then it has the potential to cause infection e.g. E. coli in a properly taken MSU. (NB do you know how to take a proper MSU? see previous, piddle in a bottle blog)
In contrast S. pneumoniae doesn’t cause infections of the pharynx and therefore if it is isolated from a throat swab then it is a coloniser as it does not have the potential to cause infection at this site. In a similar fashion if E. coli is isolated from an ulcer on the leg then it is also a coloniser as it does not have the potential to cause infection at this site.
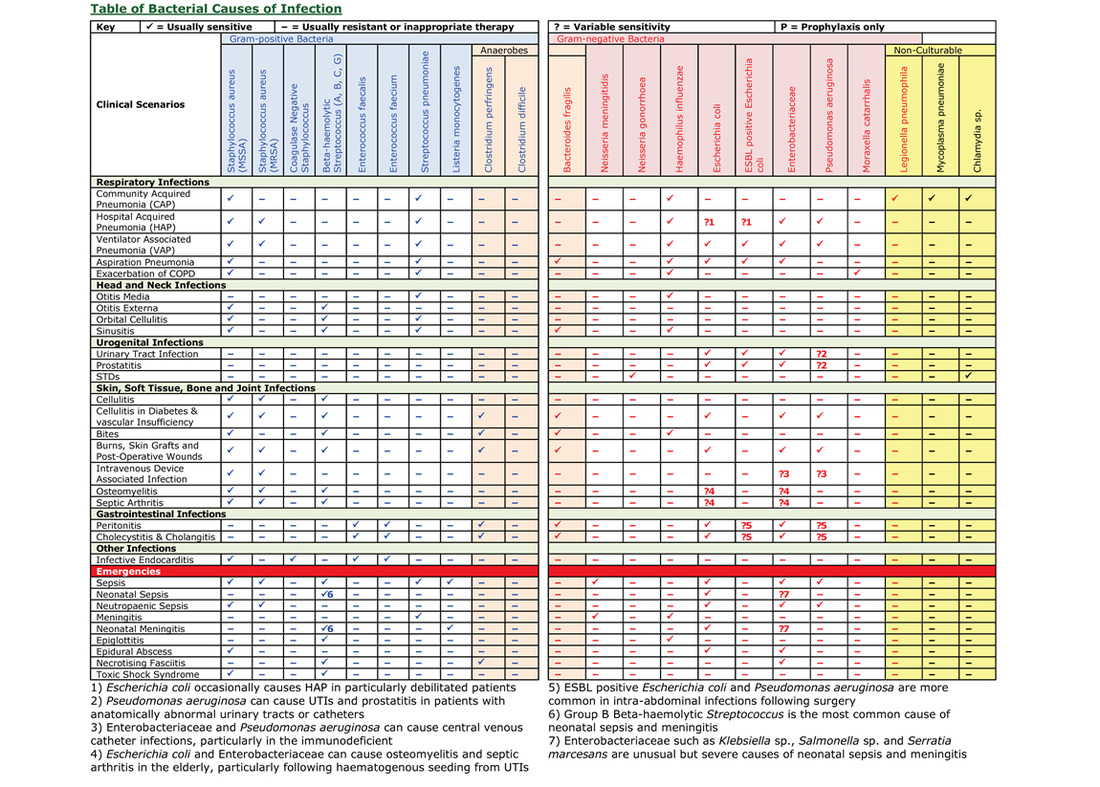
So how do you know which bacteria cause what infection? Well, you should have learnt this at University or Medical School… BUT I don’t think I really learnt this until I became a Microbiologist! So how can I help you learn this? The table below shows which bacteria are the usual causes of the common infections, and the pdf is printable as A4... it’s also in the book Microbiology Nuts & Bolts.
The five features of inflammation are: pain, swelling, redness, heat and loss of function. If inflammation or tissue destruction is absent then there is no infection, whatever bacteria you grow from the site. Remember infection is the presence of microorganisms causing damage to body tissues, if there is no damage, there is no infection.
So how do we put this all together?
If the microorganism is normal flora or doesn’t cause infection at the site from which it was isolated then it is a coloniser e.g. S. pneumoniae in the throat.
If the microorganism isn’t normal flora BUT could cause infection at the site from which it is isolated BUT there is no inflammation or tissue destruction then the microorganism is also a coloniser e.g. S. aureus from a skin wound that is not inflamed.
If the microorganism isn’t normal flora AND can cause infection at the site from which it is isolated AND there is evidence of inflammation or tissue destruction then it is probably causing an infection e.g. S. aureus in a wound that is red, painful, swollen and discharging pus. You’ll notice I said “probably”, as in this scenario it is also possible that the microorganism you have isolated is actually a coloniser and another microorganism which has failed to grow is causing the infection. The only way to work this one out is if you give suitable treatment for the microorganism you have grown and the patient doesn’t get better, then it was a coloniser all along and you need to take further samples to see if you can find the real culprit e.g. you give Flucloxacillin to treat the sensitive S. aureus but the patient doesn’t get better, when you repeat the skin swabs you now grow a Clostridium perfringens and the patient gets better when you give Metronidazole, the S. aureus was just a coloniser and the C. perfringens was the infecting microorganism.
Test Yourself
So do you know which of the following bacteria are the most likely cause of infection in each of the sites below? Infection, coloniser or normal flora? (Answers at the end of the blog)
- S. pneumoniae from pharynx from a throat swab
- S. aureus from a ulcer from a swab
- Lactobacillus spp. from the vulva from a swab
- E. faecium from the peritoneum in peritoneal fluid
- E. cloacae from the bowel in stool
- Moraxella catarrhalis from the eye from a conjunctival swab
So hopefully it is now clear. Just because you grow a microorganism doesn’t mean you have to try and kill it! Remember to love your hundred trillion bugs. Some bacteria are good for us and are part of our normal flora and some bacteria are not part of our normal flora but are doing us no harm, they are colonisers. Be nice to them… don’t throw antibiotics at them… wait for those that are causing infection then you can selectively wipe them out!
Answers
1) Coloniser 2) Infection 3) Normal flora
4) Infection 5) Normal flora 6) Coloniser



 RSS Feed
RSS Feed
