Hold onto you seats, here we go…!
Covid-19 is the name of the infection caused by the virus SARS Coronavirus 2 (SARS Cov2). It’s like pneumonia being caused by Streptococcus pneumoniae or cellulitis being caused by Staphylococcus aureus. You “catch” SARS Coronavirus 2 and “have” Covid-19.
What is SARS Coronavirus 1?
SARS Cov1 was the cause of the severe respiratory infections that occurred primarily in Hong Kong back in 2003. SARS Cov1 is different to SARS Cov2 and is not the cause of Covid-19 (see above).
How does SARS Coronavirus 2 cause disease?
The virus SARS Cov2 appears to primarily cause the alveolar epithelial cells to increase in number, leading to thickening of the alveolar wall which reduces the ability of the lungs to absorb oxygen. The infection, Covid-19, is therefore primarily a problem of low oxygen (hypoxia). A small number of patients appear to have a very severe inflammatory reaction to the virus which leads to affects throughout the body (multi-organ failure) and it is primarily these patients who require intensive care management. At present it is not possible to predict who these patients will be so we have to keep a watch on those who are unwell and in hospital in case they get worse. The majority get better though.
What are the symptoms and signs of Covid-19?
The main symptoms of the Covid-19 infection are cough and fever. Unfortunately these are not specific to Covid-19; they are in fact the symptoms of ALL lower respiratory tract infections. From a medical perspective the signs that would fit more with Covid-19 appear to be profound shortness of breath on minimal exertion and bilateral changes on chest x-ray or CT scan.
Does a negative test rule out Covid-19?
A negative test does not completely rule out Covid-19. There are number of reasons for this:
- Quality of the sample – a poor quality sample may have little viral RNA on it and so will not be sufficient to give a positive result
- Changing pattern of infection – it appears that early in the infection the virus, SARS Cov2, affects the upper respiratory tract which makes nose and throat swabs the best samples for detecting infection. Later in the infection from about day 4 onwards the infection is more in the lungs so sputum and bronchoalveolar lavage (BAL) samples become more reliable whilst nose and throat swabs become less useful
- No test is 100% perfect, all tests can have false negative results
- Currently there are no quick, easy, point of care, plug and play options…they are working on it… so no, there is no test available for GP surgeries, or “all who want it” or say we “should” have it!
REMEMBER: if you see a patient who you clinically suspect has Covid-19 BUT the test is negative then you MUST continue to treat as Covid-19.
What antivirals can I use to treat Covid-19?
At present there are no drugs that have been shown to definitely improve patient outcomes in Covid-19. Various clinical trials are on-going as part of the current pandemic. What we suspect so far is:
- Corticosteroids make Covid-19 worse – this does not include patients who are already on corticosteroids for other reasons who should definitely NOT stop their current medication
- Kaletra (Lopinavir/Ritonavir) – does not appear to make any difference to patient outcome based on latest publications. In addition many patients experience gastrointestinal side-effects such as vomiting which can increase the potential risk of transmission, as vomit includes secretions from the upper respiratory tract
- Chloroquine/Hydroxychloroquine – there are ongoing trials of this but so far evidence does not support its use outside of clinical trials
- Remdesivir – compassionate use only (from Gilead) however Gilead have temporarily shut down their website as they have been overwhelmed with requests. No clinical evidence of efficacy but there is good laboratory evidence that it may be of some benefit. Ideally it should be used as part of a clinical trial.
Is secondary bacterial pneumonia a common feature of Covid-19 as it is for influenza?
Secondary bacterial pneumonias in Covid-19 do not appear to be a big feature compared to influenza where they are a major problem. However some patients will get secondary bacterial pneumonias AND some patients will still present with bacterial pneumonias without having Covid-19 at all; good rational clinical assessment will still be needed for particularly unwell patients. The causes of secondary pneumonias will still be the usual suspects for community acquired pneumonia or hospital acquired pneumonia such as Streptococcus pneumoniae, Haemophilus influenzae and sometimes Staphylococcus aureus.
What antibiotics should I start if I suspect my Covid-19 patient also has a bacterial pneumonia?
Most patients with Covid-19 do not need antibiotics. If you do suspect a secondary bacterial pneumonia in a patient with Covid-19 then normal pneumonia antibiotics are still appropriate such as Amoxicillin, Clarithromycin and Doxycycline.
Can SARS Coronavirus 2 cause Hospital Acquired Pneumonia (HAP)?
Any respiratory virus can cause HAP including SARS Cov2. Any patient who develops HAP in the current pandemic should be evaluated for Covid-19 and infection control precautions implemented.
The current test for Covid-19 detects current infection. It is not 100% reliable (see above) and it doesn’t tell you whether the HCW has previously had Covid-19. There is no value in using the current test to screen HCW or manage the hospital workforce who have no symptoms, but there may be a value in testing any symptomatic contacts of healthcare workers to see if the healthcare worker has been exposed to Covid-19 or not. If the HCW has not actually been exposed to Covid-19 then they can probably return to work, although as no test is 100% reliable there may be instances where this leads to someone returning to work who has actually been exposed. This may be a necessary risk if hospitals start to run out of staff!
In the future there is likely to be a serology test that detects past infection and this will be very useful for managing the workforce.
Should healthcare workers with symptoms be tested?
At present we are not testing HCW who are symptomatic. It is likely that this will change in the future as the capacity for testing increases because if someone can be shown to have had a mild case of Covid-19 then the NEXT time they have mild upper respiratory symptoms it can be assumed they are already immune and the new symptoms are NOT Covid-19 and they can still work in some capacity in healthcare even if not with direct patient contact.
Where do the 7 day and 14 day self-isolation figures come from?
- If you have Covid-19 then you are infectious for 7 days after your symptoms start and hence you need to self-isolate for 7 days.
- If you are exposed to someone with Covid-19 then the incubation period (the time it takes for you to develop symptoms) is up to 14 days; so if you haven’t developed symptoms by 14 days then you have either not been infected OR you have had a mild infection; either way you no longer need to self-isolate.
Being tested for coronavirus is not needed if you’re staying at home.
Can you catch SARS Cov2 again and get Covid-19 again?
Based on what is known about other coronaviruses, infection with SARS Cov2 (and hence Covid-19 infection) will give immunity that will prevent catching SARS Cov2 again over the short term (probably about a year). In addition future infections in later years are likely to be much milder as these infections will essentially “boost” the immune system that has already been primed by the first infection and the person will handle the virus much better. Over time SARS Cov2 is likely to become yet another cause of the common cold we see every year, with only mild symptoms, and we won’t even know we’ve had it, well as long as the economy recovers!
How long can SARS Coronavirus 2 last on surfaces?
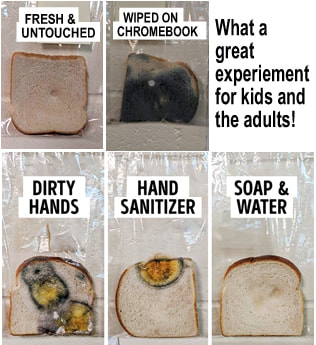
SARS Cov2 can survive as infectious material on surfaces for quite a while but it does depend on the surface material. The virus survives longer on plastic and metal than cardboard and paper, but in either case it lasts for hours, which is long enough for it to potentially infect someone else. The key message is wash your hands regularly and whenever you have been in contact with a potentially contaminated surface and if body fluids contaminate a surface then clean the surface before washing your hands. SARS Cov2 does not survive for days on surfaces and will quickly die off. Although cleaning “touch surfaces” is helpful, it is of much greater importance and responsibility to wash your own hands.
What are Aerosol Generating Procedures (AGPs)?
AGPs are procedures that might generate small particles of suspended material which may then be inhaled, exposing people in close proximity to infectious material. There is a lot of debate as to whether Ear Nose and Throat (ENT) procedures should be classified as AGPs… I personally think they probably are! The current list of AGPs includes the following but this may change:
- Intubation, extubation and related procedures;
- Tracheotomy/tracheostomy procedures;
- Manual ventilation;
- Open suctioning;
- Bronchoscopy;
- Non-invasive ventilation (NIV) e.g. Bi-level Positive Airway Pressure (BiPAP) and Continuous Positive Airway Pressure ventilation (CPAP);
- Surgery and post-mortem procedures in which high-speed devices are used;
- High-frequency oscillating ventilation (HFOV);
- High-flow Nasal Oxygen (HFNO)
- Induction of sputum
- Some dental procedures (e.g. high speed drilling).
What Personal Protective Equipment (PPE) do I need to wear in hospital and why?
When caring for most patients with Covid-19 the current PPE is a surgical face mask, plastic apron and gloves. This prevents “unintentional” contamination e.g. you are rolling a patient for care needs and they cough; the initial aim was not to roll the patient to treat their chest, as chest physiotherapy is “induction of sputum” (see above). For AGPs (see above) the PPE is FFP3 face mask, long sleeved disposable gown, gloves and disposable eye protection. A good summary page can be found on the Public Health England website here.
The main risk factors for severe infection include:
- Increasing age, especially over 70 years
- Cardiovascular disease
- Diabetes mellitus
- Chronic respiratory conditions e.g. chronic obstructive pulmonary disease (COPD), cystic fibrosis (CF), brittle asthma
- Hypertension (high blood pressure)
- Immunosuppression e.g. cancer, chemotherapy, neutropaenia
Note: probable co-morbidities based on other respiratory viral infections include: obesity, smoking and chronic kidney disease
Why do I keep hearing about Angiotensin Converting Enzyme (ACE) inhibitor drugs in relation to Covid-19?
SARS Cov2 uses the ACE2 receptor on human cells to get inside the cell and cause disease. During the SARS Cov1 epidemic in 2003 it was suggested that blocking ACE receptors may prevent or improve infection… however it didn’t. It turns out that ACE inhibitor drugs usually block ACE1 receptors, not ACE2, and so have no benefit. Note: [Correction] ACE inhibitor names end in “pril” e.g. Lisinopril, Captopril, Enalapril (oops, thanks Anita for spotting the mistake!).
Why is there a concern about the use of Ibuprofen in Covid-19 and is it real?
Ibuprofen has been shown in experiments to increase the production of ACE2 receptors on human cells, so in theory, it might predispose to infection with SARS Cov2. However there is no evidence that this makes any difference in real terms. The WHO has taken the precautionary step to recommend that people infected with SARS Cov2 don’t take drugs like Ibuprofen but it just a precaution, nothing more. If you are taking Ibuprofen for other health reasons, e.g. arthritis, then you should probably continue to take it, it’s a theoretical risk not a proven risk.
When can we realistically expect a vaccine?
The fastest that anyone is likely to get a vaccine against SARS Cov2 onto the market is about 18 months. They can make a vaccine faster (6-8 weeks in theory) BUT it must go through clinical trials to make sure it is safe and effective and this takes a long time. Don’t expect to see a vaccine until the end of 2021 at the very earliest.
What really is the mortality for Covid-19?
No one knows. All of the data and statistics being produced around the World are based on the figures of who is being tested and this is skewed to severe infections. At present in the UK we are only testing patient’s sick enough to be admitted to hospital with severe respiratory infections. We are not testing everyone who’s admitted (see above). Obviously the mortality will be higher in these patients than people who have mild symptoms and are well enough to stay at home. There is also an increasing body of evidence to suggest that a large number of people are almost completely without symptoms (up to 90% if you believe some of the data coming out of Italy). If that’s true then the mortality is at least 10 fold lower than currently being quoted; so about 0.1-0.3% rather than 1-3%... we’ll only know the truth after this has all settled down.
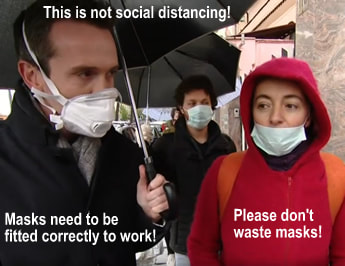
I am not a healthcare worker or patient in hospital; do I need to wear a face mask?
There is no evidence that wearing a face mask outside of the healthcare setting makes any difference to whether you will get an infection or not. Respiratory viruses are spread by large droplets which settle out of the air very quickly. The most important factor in preventing the spread of this type of virus is washing your hands so you don’t pick the virus up and then touch your face. As long as no one coughs directly in your face a mask offers no additional help; in hospitals we are looking after people who have this infection and might cough at us so we do need to use face masks. In fact for most people wearing a face mask it isn’t fitted correctly and isn’t very comfortable; those wearing them tend to touch their faces more, so might actually make themselves more likely to become infected!
Gloves are not a substitute to washing your hands, and most of the time wearing them makes people complacent. On many occasions I have seen people wearing gloves touching their faces, using their mobile phone, drinking drinks and even eating food. In hospital we wear gloves for short periods of time, remove them when we have finished what we are doing and take extra care to wash our hands (even when we have used gloves). Hands get hot and sweaty with prolonged use of gloves and this leads to increased proliferation of bacteria as well as poor skin integrity. Outside of healthcare there is no need to wear gloves; just wash your hands.
Should I use hand sanitizer to clean the door handle, ATM button or the lock on my allotment gate etc.?
Hand sanitizers are for use on hands… the clue is in the name. They are not for cleaning surfaces and have almost certainly never been tested to see if they are effective in this situation. Don’t use them for something they’re not meant for, at the very least they just won’t work and at worst they make you think they are more effective than they are. If you are worried about touching a surface then wash or sanitize your hands afterwards… but don’t smear stuff all over the door handle the build-up of “gunk” just makes it worse for everyone else. Note: if using hand sanitiser, use it properly! It’s not to rub into your fingertips… your whole hand surface needs to be covered; if in doubt use soap and water.
Try this at home, place a slice of bread in a plastic food bag after pressing your hands onto its surface and see what grows! … A teacher, Jaralee Metcalf, came up with this idea for her class and it's brilliant...
Social distancing is the phrase adopted to describe keeping a 2 metre (6 foot) gap between yourself and others. The reason for this is that large droplets containing virus produced by someone coughing out SARS Cov2 will fall to the ground within this “separation” distance and not contaminate anyone else. If you maintain this distance then it helps prevent the spread of the virus. Add in washing your hands and staying at home and you are doing ALL that you can to help reduce the spread of the virus. Healthcare workers thank you for implementing these measures to protect us and those at greatest risk.
It is unlikely that SARS Cov2 came from actually eating unusual meats like snake. SARS Cov2 is a bat coronavirus affecting the bat gastrointestinal tract, and is likely to have been acquired through contact with bat guano (poo!). Another good reason to wash your hands!
Can I still kiss and cuddle my loved ones?
You are welcome to do what you like but it would be prudent not to kiss and cuddle someone who has symptoms and signs of Covid-19… but let’s be real, if you already live with this person you are already exposed! If you are in a high risk category then try to avoid coming into close contact with loved ones, e.g. separation and care in shared spaces within the home such as kitchens, bathrooms and sitting areas. On a related note, I heard a prediction that there will be a baby boom in 9 months’ time (this often happens after a crisis) and marketing people are already coining the phrase “Coronials”.
REMEMBER if you have Covid-19 you must self-isolate for 7 days. Call a neighbour, friend, family member or a Covid-19 volunteer to assist you with basic needs. It would be good to have a central number for you to call but as yet I haven’t seen such a resource! Therefore if you can, pop a note with your contact details through your neighbours doors; if you have to go out, offer to shop for them too.
Will exercise help me now?!
There appears to have also been a run on gym equipment (Editor Chief in Charge is guilty of this!) Not sure if this is panic buying or last minute attempts to get healthy but I suspect it is more to do with gyms being closed and none of us gym addicts being able to get our fixes unless we do “home-gyming”. Going for exercise outside is currently allowed however a sudden increase in exercise will not provide protection; large increases in exercise when your body has not adapted to exercise may also not be beneficial.
I am also slightly concerned that all of those who went out and panic bought all of the high carbohydrate foods (pasta, bread flour, rice) over the last couple of weeks will actually eat all of that food and the obesity epidemic in the UK will get worse as a result of Covid-19… but then I’m a cynic who’s worried whether he’ll get an Easter egg this year or not… (Hint, hint to Editor Chief in Charge …AKA Wife)
Can the Easter Bunny get covid-19!?!
NO! Don’t even go there! Nor can pets including cats and dogs… Note: bats do not appear to be affected themselves by the virus they carry. I am expecting a really big egg after all of this! (Editorial contribution: I’ll buy you an ostrich!)
Remember these 2 key rules for dealing with Covid-19:
- Keep 2m of social distancing, wash your hands and stay indoors!
- If all else fails remember rule number 1
“Keep your head when all around you are losing theirs” or as I like to say “Stay Sane!”
(Apologies to Rudyard Kipling)


 RSS Feed
RSS Feed
