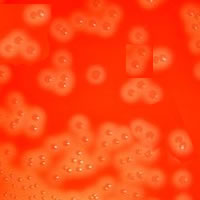
yesterday when you notice that something doesn’t quite add up. The growth on the blood agar looks like an Alpha-haemolytic Streptococcus but the Gram film from yesterday looked like a Staphylococcus (Gram-positive coccus in clumps). To make matters more confusing the bacteria have not grown on the ISO sensitivity agar either.
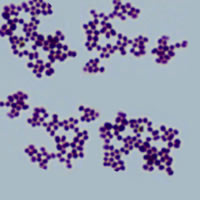
profile index) test for Streptococcus spp. but this doesn’t identify the bacteria. The colonies of the “alpha-haemolytic streptococcus” on the blood agar are Gram stained and instead of a Gram-positive coccus in chains, as you would
expect from a streptococcus, the organism is definitely forming clumps.
Have you ever been in this situation? What would you do next? If the answer is to issue some vague report and move on to the next sample then think again, and consider the following patient...
A lady in her 80s presents to the hospital with a history of
increasing tiredness and weight loss associated with low grade fevers. She is also complaining of dysuria. Her primary care physician has done some initial blood tests and sent two urine samples to the microbiology laboratory, and has
empirically treated her for a UTI with Trimethoprim followed by Ciprofloxacin, but with no success. The patient has a slightly raised white blood cell count and C-reactive protein but otherwise her blood tests are unremarkable. Her urine
samples had raised white blood cells in them but were reported as no significant growth.
This patient is clearly unwell, and not identifying the isolate
is not an option, so what are the next steps?
The antibiotic sensitivity tests can be repeated on a more
nutritious agar such as ISONAD, and this will probably show that the organism has good zones of inhibition to antibiotics such as the Beta-lactams, including Amoxicillin, and the glycopeptides, such as Vancomycin, but is resistant to the
quinolones, including Ciprofloxacin.
If you have no other identification methods available to you
then this is probably the limit to what can realistically be achieved in your laboratory and you may need help from a Reference Laboratory to identify the bacterium further. However, if you have MaldiTOF (Matrix-assisted laser
desorption/ionisation time of flight) mass spectrometry available then the next step would be to put the bacterium through this. In this case the bacterium is likely to be identified as Aerococcus urinae. Aerococcus urinae is a
Gram-positive coccus which forms clumps, looks Alpha-haemolytic on blood agar and does not grow on ISO sensitivity agar...weird huh!?
Infections with Aerococcus urinae have increased dramatically over the last couple of years which has lead to it being described as an emerging pathogen. However, there is another possible explanation. Due to the availability of technology such as MaldiTOF the identification of bacteria in
routine diagnostic microbiology laboratories has improved dramatically.
Let me explain further. MaldiTOF is cheap, quick and easy to
perform. It is very simple for a BMS to put a bacterial isolate through the system to get a name out of the other end. Tad-da! Previously, identification was time consuming and relatively expensive, with overnight incubation and difficulty with reading the results, not to mention the fact that API systems do not identify Aerococcus spp. As a result, Aerococcus spp. would only previously have been identified if they had grown in a blood culture or other sterile site, and often perhaps not even then. In other samples they would have been called Alpha-haemolytic Streptococcus sp. and a comment made that they failed to grow for identification. For certain they would have been present in the samples; we just would not have known what they were.
So does our new found knowledge help patients? Well, yes it does.
Firstly, Aerococcus urinae (as its name suggests) is a significant cause of infection of the urinary tract and so our lady does indeed have a UTI. However, as they are not
recognised in urine cultures they are often missed and patients end up with chronic infections which are treated more by luck than judgement.
Secondly, Aerococcus urinae also tends to be resistant to the
antibiotics Trimethoprim and Ciprofloxacin, both commonly used to treat UTIs. Patients often only start to feel better if given active antibiotics such as Amoxicillin or Nitrofurantoin.
Thirdly, Aerococcus urinae tends only to cause UTIs in the
presence of significant urinary tract pathology such as incomplete emptying of the bladder or bladder lesions such as cancer. It is therefore suggested that all patients with UTI due to Aerococcus spp. should be investigated for an
underlying urinary tract abnormality.
Finally, Aerococcus spp. are significant when found in blood
cultures as they usually indicate a diagnosis of infective endocarditis. All patients with this type of infection should have echocardiography and empirical treatment for infective endocarditis. The current recommendation is to treat with a combination of antimicrobials such as Amoxicillin and Gentamicin as for Enterococcal endocarditis (the 2 bacterial species behave in a similar manner and have similar sensitivity profiles).
Our patient with tiredness, weight loss and low grade fevers was found to have infective endocarditis and a bladder diverticulum which prevented her bladder emptying properly. After 4 weeks of antibiotics and surgical correction of the bladder problem she made a full recovery.
So the key messages about Aerococcus urinae infections are:
- Aerococcus urinae is a significant cause of UTI (3%)and infective endocarditis (>90% if seen in blood
culture) - Treatment of Aerococcal UTI should ideally be with
Amoxicillin OR Nitrofurantoin - Treatment of Aerococcal infective endocarditis should be with Amoxicillin PLUS Gentamicin
- Aerococcus is probably not an emerging pathogen, our
diagnostic tools have just improved and we now recognise it for what it is (a Gram-positive coccus in clumps which grows like an Alpha-haemolytic
Streptococcus) – put it through the MaldiTOF it's probably an Aerococcus sp. ...go on keep investigating...see if I’m right.
 RSS Feed
RSS Feed
