Many patients have to start empirical treatment with antifungals whilst awaiting results from reference laboratories as there is often a lack of locally available diagnostic tests. This results in a lot of unnecessary treatment of patients with potentially toxic and expensive drugs. In fact, antifungals are often the most expensive drugs used within hospitals; using better diagnostics could produce significant cost savings. To give you an idea, the listed drug costs in the BNF for one day of antifungal treatment for a 70kg patient are:
- IV AmBisome (5mg/kg OD) = £700
- IV Caspofungin (50mg OD) = £330
- IV Voriconazole (4-6mg/kg BD) = £300
- Microbiology best practice
- Histopathology best practice
- Radiology best practice
I’m not going to list all the recommendations here as I haven’t mushroom! (ha ha). However, I’ll give an overview here, the full guideline can be found here but unfortunately it is not free to access (a personal bug bear of mine, I believe national societies that produce guidelines should make them freely available, see previous blog!!)
The emphasis for microbiology recommendations are on fast turnaround and accurate identification of a fungus from different types of clinical specimens. The recommendations state specific conditions where testing is effective and where it is of no value.
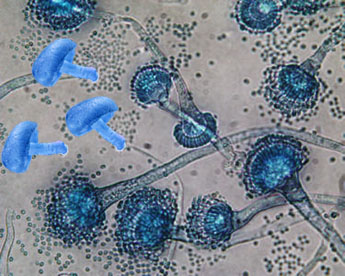
1. Microscopy to see fungal hyphae
This rapid test can potentially confirm the presence of fungi within a few hours. However, in the hands of a skilled biomedical scientist it is also possible to distinguish different types of yeasts (Candida spp., Cryptococcus spp., dimorphic fungi) as well as tell the difference between septate (Aspergillus spp.) and non-septate moulds (Zygomycetes) which can further influence the correct choice of antifungal treatment.
- Used for specimen types: any specimen type
- Advantage: the presence of fungi in normally sterile samples is always significant, so biopsy should be encouraged whenever possible
- Disadvantage: many samples are not actually from sterile sites, or have to be taken through non-sterile sites, and therefore the presence of fungi may indicate colonisation or contamination instead of infection. For example, in immunosuppressed patients with a diagnosis of fungal sinusitis, the sensitivity of microscopy and culture on Bronchoalveolar lavage (BAL) samples is only about 50% whereas it is 78% for sinus biopsy samples.
2. Microscopy by direct immunofluorescence
This rapid test can potentially confirm the presence of Pneumocystis jirovecii, the cause of PCP, within a few hours.
- Used for specimen types: Sputum or BAL. If a BAL cannot be done then it is recommended to take at least 3 separate sputum samples in order to try and improve the sensitivity
- Advantage: high sensitivity of 86-97%
- Disadvantage: PCR is said to be even more sensitive however PCR costs more and takes longer
3. Fungal culture
This is not a rapid test but can confirm the presence of fungi in a wide variety of clinical specimens.
- Used for specimen types: any specimen type
- Advantage: allows antifungal sensitivity testing to be done. It is recommended that the fungus is saved for at least 3 months in case the patient fails therapy and therefore antifungal sensitivity is required
- Disadvantage: it can take up to 14 days (21 days for CSF) to detect any slow growing species of fungi. If the fungus wasn’t saved, antifungal sensitivity testing is not possible
4. Detection of antigens
These are rapid tests that can potentially confirm the presence of fungi within a few hours. Different fungi are detected by the presence of parts (antigens) of the fungi. Three main tests are recommended Cryptococcal antigen, Galactomannan and 1,3-beta-D-glucan depending on causative fungi
- Used for specimen types: various specimen types depending on test
- Advantage: specific to fungi (bacteria and viruses do not react in the test)
- Disadvantage: not very sensitive and therefore prone to false negatives (negative test result but the patient does have the disease)
Cryptococcal antigen (CRAG) is a cell wall antigen released by Cryptococcus spp. into CSF and serum. CRAG is the antigen being looked for as well as the name of the test. A positive test for CRAG in CSF or serum from an HIV positive patient has a high sensitivity and specificity for Cryptococcus spp. infection including cryptococcal meningitis.
Galactomannan is a cell wall antigen released by Aspergillus spp. Galactomannan is the antigen being looked for as well as the name of the test. It can be detected in blood and BAL samples from patients with invasive aspergilossis. A value of 0.5 is considered positive in blood, a value of 1.0 is considered positive in a BAL. Some doctors use Galactomannan to screen patients for aspergillosis but this is potentially misleading. If the incidence of aspergilossis in the population being screened is low then a positive test is more likely to be a false positive, whereas if the incidence is high then the positive result is more likely to be a true positive. The recommendations indicate that if the prevalence is 5% in the population tested then the positive predictive value of a positive Galactomannan is only 31%, whereas this increases to a PPV of 69% if the prevalence is 20%. What this means in practice is that the test should be reserved for high-risk patients (bone marrow transplant recipients, acute myeloid leukaemia and aggressive chemotherapeutic regimens) where a result of >0.5 gives a sensitivity of 78% and a specificity of 81% when these patients are neutropaenic which is when they are most likely to be tested anyway.
1,3-beta-D-glucan (BDG) is a cell wall antigen released by a number of fungi including Aspergillus spp., Candida spp., and P. jirovecii. It is not present in Cryptococcus spp. or the Zygomycetes. BDG is the antigen being looked for as well as the name of the test. BDG is prone to false positive results; however it does have a good negative predictive value and is therefore useful in excluding invasive fungal infections with Aspergillus spp., Candida spp., and P. jirovecii. It is particularly helpful in diagnosing PCP when a BAL or sputum sample can’t be taken for some reason.
5. PCR The guideline does not recommend the widespread use of PCR in isolation for most fungi as there is insufficient data except for PCP PCR on respiratory samples; this is the most sensitive and therefore recommended test for PCP. However, it does recommend combination testing combining PCR for Aspergillus spp. with Galactomannan or BDG. If all three tests are negative then invasive aspergillosis can be excluded. The most predictive result is a positive Galactomannan and PCR which indicates invasive aspergilossis and treatment should be started as soon as possible. The problem occurs when a patient is positive in only a single test in which case further investigations would be required to reach a diagnosis. Histopathology and radiology can be very helpful in this situation.
Histopathology best practice
The guideline recommends that specialised fungal stains including Grocott methenamine silver (GMS) stain and periodic acid-Schiff (PAS) should be performed on all samples received by histopathology laboratories from patients with suspected invasive fungal infections. These stains enhance the appearance of fungi and make them easier to see. An experienced Histopathologist can also distinguish the different types of fungal species; the guideline provides an excellent detailed description of the morphological characteristics of the different fungal species in histopathological specimens.
Radiology best practice
The guideline recommends radiological investigations for specific clinical presentations:
- CT is the recommended investigation for pulmonary infections in immunosuppressed patients who develop a fever as well as a cough, shortness of breath, chest pain or respiratory failure or patients who have a continuously raised Galactomannan or BDG. In these cases there should be a low threshold for imaging and this should be performed within 48 hours of the onset of new respiratory symptoms or a fever that lasts for more than five days despite antibacterial therapy. The typical features of fungal infections on CT are nodules >1cm for moulds and ground-glass shadowing for PCP, although other appearances can also occur e.g. consolidation
- MRI with gadolinium is the recommended investigation for fungal sinusitis and central nervous system infections because it is better than CT for detecting soft tissue inflammation and abscesses. It is important to remember that cerebral aspergilossis can present as a cerebral infarction or haemorrhage because the fungus is angioinvasive; it likes to invade along blood vessels causing them to clot or bleed.
Summary
Invasive fungal infections are uncommon and difficult to diagnose, as a result there is often a delay in starting patients on appropriate treatment. There is also a cost to treating patients empirically while waiting for results to become available both the potential toxicity to the patient and the expense. The new guideline published in April’s Lancet Infectious Diseases by the British Society for Medical Mycology is excellent, providing clear recommendations for how we should be diagnosing invasive fungal infections. What’s more the guidelines are specific enough that we can audit current practice against their recommendations in order to identify where we can improve practice…my only wish is that these guidelines were made freely available and therefore could be accessed by a wider audience.
 RSS Feed
RSS Feed
