In the UK, there are on average 1,600 cases and 7 deaths per year. It is not particularly common therefore it is easily missed. Any patient/returned traveller who has visited an endemic country (see map) who presents with a fever and flu-like symptoms should have malaria on the differential diagnosis for what might be causing their illness.
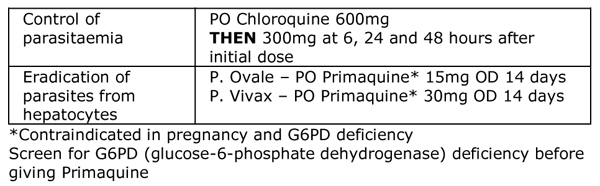
ovale rather than the typical Plasmodium falciparum, and we had to remind ourselves of the treatment for P. ovale.
There are 5 species of malaria which can infect humans:
• Plasmodium falciparum (most common and most deadly)
• Plasmodium vivax (benign)
• Plasmodium malariae (benign)
• Plasmodium ovale (benign)
• Plasmodium knowlesi (rare - only found in some forested areas of South-East Asia)
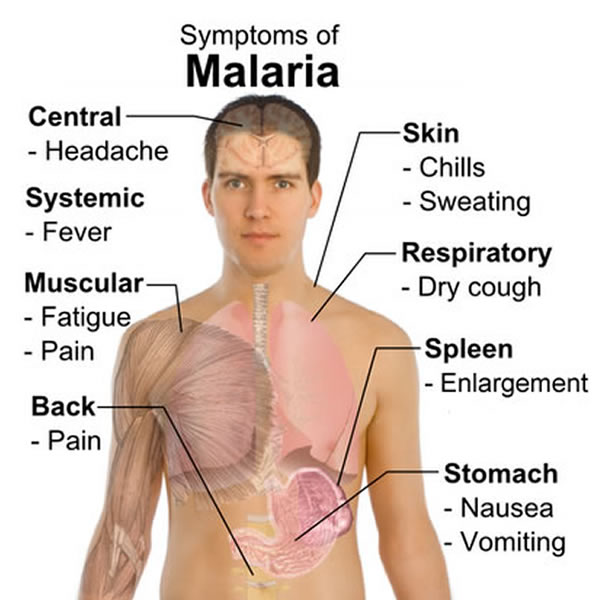
Clinical
P. falciparum and P. knowlesi have an incubation period shorter than 1 month and can cause severe disease (presence of complications such as high parasite load >2%, cerebral malaria, pulmonary oedema, severe anaemia, hypoglycaemia, uraemia and lactic acidosis). The benign malarias (P. ovale along with P. vivax and P. malariae) usually result in a milder disease of a flu-like illness. These species can have an incubation period of longer than 1 month as they can reside in the liver and reactivate.
Many laboratories now use a combination of a malaria antigen test on whole blood samples followed by microscopy of thick and thin blood smears to distinguish the different types of malaria.
• Antigen tests are good for diagnosing malaria (especially in laboratories that do not see a lot of malaria), but they cannot always distinguish between different species nor do they give a parasite load. They are valuable in laboratories that do not see malaria frequently as they are quick, easy to perform and sensitive. Antigen tests should be used in combination with microscopy.
• Microscopy gives the specific species of malaria and a
parasite load which helps decide on severity and risk of complication. This test requires a high degree of expertise and experience which is difficult for laboratories in the UK to maintain as they do not see enough positive malaria tests.
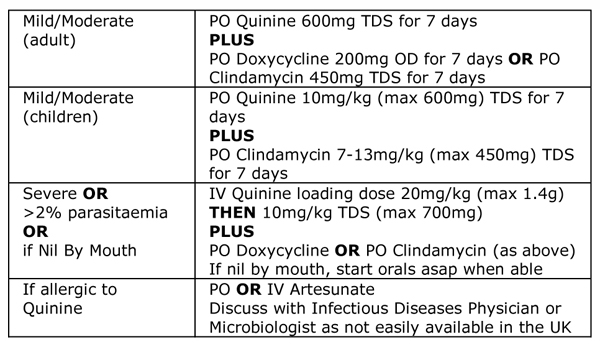
Treatment
The treatment of malaria depends on the malaria species and the severity of illness. If the species is not known then the patient should be treated as though they have falciparum malaria as this is the most dangerous.
the community under a general practitioner. It is aimed at controlling the parasitaemia (the amount of parasite in the blood stream) and then eradicating the parasite from the hepatocytes (liver cells). P. malariae does not tend to relapse because chronic infection of liver cells is uncommon.
Treatment of adults is shown in the table below and is based on the British Infection Society Guidelines for the Treatment of Malaria 2007. For the treatment of children seek specialist advice from an Infectious Diseases Consultant and use the Children’s British National Formulary.
not catch it in the first place!


 RSS Feed
RSS Feed
